
1
Fifth stage
Gynecology
Lec-6
د.سراب
9/3/2016
Conditions affecting the vagina and vulva
Anatomy:
The vulva is the term used to describe the external female genitalia – the sexual
organs.
It includes the labia majora and minor, clitoris and fourchette.
The vulval vestibule is defined anatomically as the area between the lower end of the
vaginal canal at the hymenal ring and the labia minora.
The different anatomical areas of the external genitalia have different histological
characteristics and embryological origins.
Both the labia minora and majora are covered with keratinized, pigmented,
squamous epithelium.
The labia majora are two large folds of adipose tissue covered by skin containing hair
follicles, sebaceous and sweat glands.
In contrast, the labia minora are devoid of adipose tissue and hair follicles, but
contain sebaceous follicles.
The normal vulval vestibule is covered with non-keratinized, non-pigmented
squamous epithelium and is devoid of skin adnexa.
Within the vulval vestibule are the ducts of the minor vestibular glands, the
periurethral glands of Skene, the urethral meatus and the ducts of the Bartholin’s
glands.
The Bartholin’s glands (major vestibular glands) are the major glands of the vestibule
and lie deep within the perineum.
Both the major and the minor vestibular glands contain mucous-secreting acini with
ducts lined by transitional epithelium.
The ducts of the Bartholin’s glands exit at the introitus just above the fourchette at
approximately five and seven o’clock on the perineum and those of the minor
vestibular glands are distributed throughout the vulval vestibule.
The vagina and vulva are commonly known as the lower genital tract with the vagina
leading to the upper genital tract (uterus, cervix, tubes and ovaries).
The vagina has is a tubular structure but has anterior and posterior walls which lie in
opposition.
Vulval skin has different physiological properties when compared to other regions of
the body such as the forearm.
2
Transepidermal water loss is twice the amount in vulval skin compared to forearm
skin.
This suggests that the stratum corneum, the protective layer of vulval skin, functions
poorly as a skin barrier when compared to other skin areas and may explain why
vulval skin is more prone to irritancy.
Assessment:
History:
A full history and clinical examination (with optional vaginal swabs and biopsies) are
essential to make the diagnosis.
Vulval skin is an extension of general skin surfaces and it is important in the history to
ask about general skin problems as this might point towards the diagnosis, for
example psoriasis or eczema can synchronously affect the vulva and the limbs.
The history should focus on the presenting complaint.
It is important to discuss current methods of skin care (e.g. use of scented products
which can aggravate symptoms), which topical treatments are being used (e.g. some
creams such as antifungals can aggravate the problem) and the impact of the
symptoms on sexual functioning.
Examination:
The clinical examination should include all skin surfaces and the vulval area should be
examined systematically with a good light source.
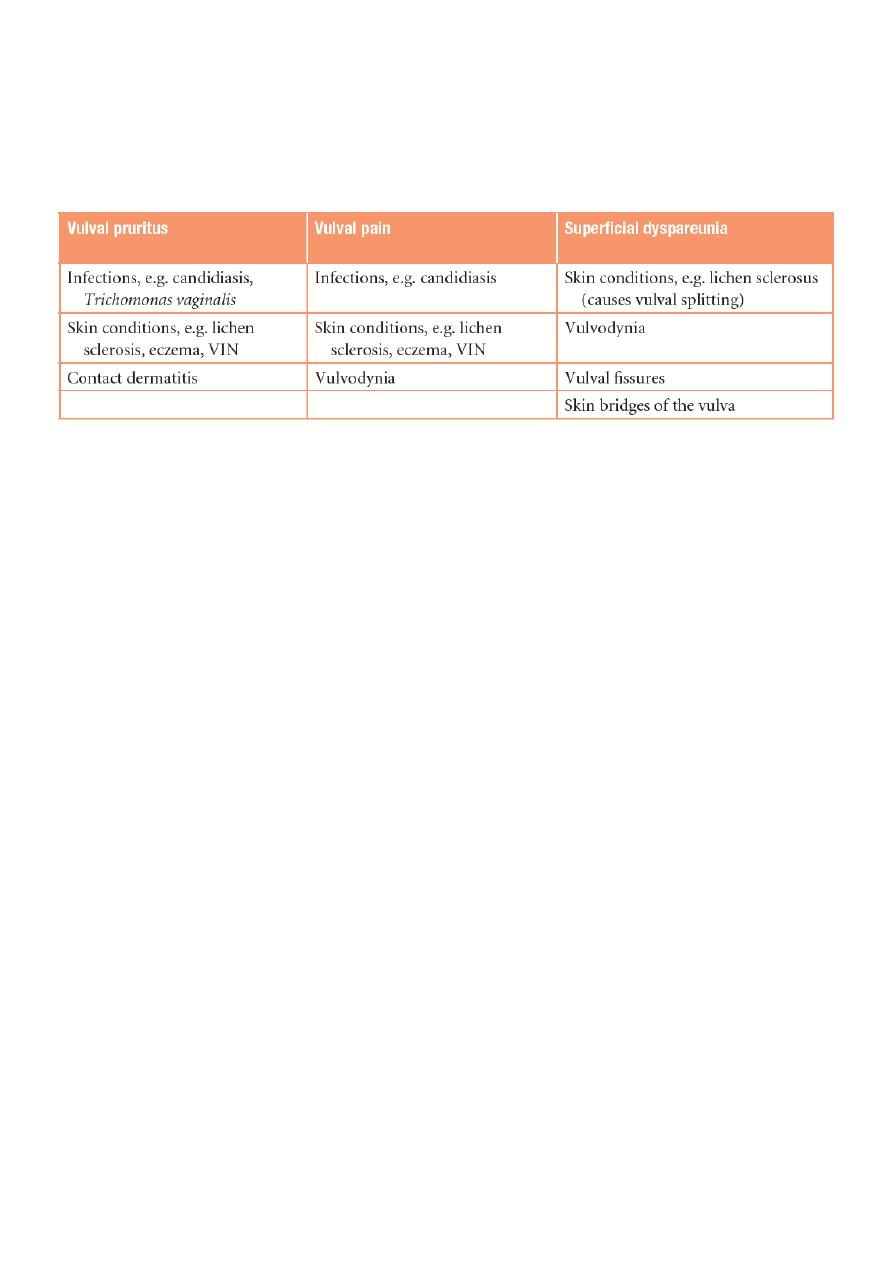
Vulval pruritus, pain and superficial dyspareunia are common symptoms and Table
15.1 illustrates the differential diagnoses of different symptoms, although this is not
an exhaustive list.
Confusingly for the clinician, most patients have more than one symptom.
After a full history and clinical examination, it should be possible to make a
provisional diagnosis.
Investigations:
Sometimes it is necessary to carry out some swabs and a biopsy for confirmation.
Microbiological swabs may be indicated to exclude infection as a cause of vulval
symptoms (e.g. candida and Trichomonas vaginalis can cause vulval itching, herpes
simplex may cause vulval ulcers).
When there is a lesion on the vulva and the diagnosis is unclear, then an outpatient
vulval biopsy is helpful. The Keyes punch biopsy is a 4-mm sample of skin that can be
taken under local anaesthetic in the clinic.
3
A pathology sample allows an accurate diagnosis to be made and the correct
treatment to be instigated. Biopsies should be carried out when there is a pigmented
lesion, a raised or indurated area and a persistent ulcer.
Differential diagnosis of vulval complaints:
Treatment principles
:
Treatment should be given based on a correct diagnosis and empirical treatment
should be discouraged because of the potential side effects of treatment.
Good skin care of the vulva is essential, with an avoidance of scented and over-the-
counter products as these can produce unnecessary irritancy on the skin.
Emollients are bland scent-free topical products that can soothe and rehydrate the
skin and can be used liberally, for example aqueous cream.
When prescribing cream, for example steroid ointments, it is important to be clear to
patients how much, when and where to apply the treatment.
Patients value showing them the application of the ointments or creams in the clinic.
Dosage is important particularly when prescribing steroids. One finger-tip-unit of
cream or ointment is from the last crease in the index finger to the tip and equates to
0.5 g.
A 30-g tube when used twice a day therefore should last for a month.
Causes of vulvar conditions:
Infection: candida, Trichomonas vaginalis.
Inflammation: Lichen planus, Lichen sclerosis.
Trauma: sexual or asexual.
Drugs.
Premalignant and malignant conditions.
Autoimmune: Crohn's disease, Paget's disease.
4
Infections:
Candida infection:
Candida albicans dimorphic yeast.
Symptoms pruritus, vaginal discharge (white, cheesy, adherent to vaginal skin).
Signs redness, erythema, swelling, macerated skin.
Investigation swab.
Treatment symptoms control (give alarmin for pruritus), local care, antifungal
(local and systemic).
Trichomonas vaginalis:
It is protozoa, consider as STD.
Symptoms pruritus, discharge (green gray, frothy), soreness which lead to
dyspareunia.
Signs redness, swelling, strawberry lesion of vagina and cervix (2% of patients).
Investigation wet smear (saline).
Treatment for patient and husband, screening for other STD, metronidazole for 2
weeks, local care.
Herpes simplex:
Genital herpes caused by HSV-2 and increasingly by HSV-1 (due to oro-genital
sex).
There is primary and recurrence phases of infection.
Primary is most severe.
Symptoms pain, ulcer, dyspareunia, retention of urine, systemic manifestation
(fever, tired).
Signs multiple small elevated ulcers, swelling, erythema.
Investigations swab.
Treatment local care, analgesia, normal saline path, acyclovir.
Recurrent infection less severe and it is prolonged by stress, fever, sexual
intercourse, menstruation.
Human papilloma virus:
Condition called condyloma acuminatum (DDx: condyloma lata).
Presentation skin lumps different in size.
Treatment medical or surgical.
5
Other infections:
Syphilis.
Lymphogranuloma venereum.
Inflammatory:
Lichen sclerosis:
Inflammatory destructive skin valvar condition.
Could be associated with other skin lesions.
Cause is unknown but it could be autoimmune.
In young self-limited.
In elderly premalignant condition, destructive, not self-limited.
At beginning (erythema, ecchymosis) then (fissuring) then (scaring).
Signs narrowing of vaginal opening lead to dyspareunia, scaring of labia minora,
amputation of citreous.
Investigations biopsy (indications erosion, pigmentation, persistent ulcer).
Treatment:
o Valvar care: barriers, path.
o Local steroids (long term) gradual rate increase.
o Follow up (because it is premalignant).
o Rarely need surgery (if narrowing not improved by steroid.
Lichen planus:
Autoimmune condition.
Other associated autoimmune diseases pernicious anemia, type1 DM, thyroid
diseases, Addison's disease.
Associated with other skin conditions.
Symptoms pain, itching, dyspareunia, apareunia, bleeding (post-coital).
Signs velvety, Koebner's phenomenon.
Investigation biopsy for histopathology (indications erosion, pigmentation,
persistent ulcer).
Sometimes it involved the upper respiratory tract, esophagus, external auditory
meatus.
Treatment steroid, valvar care.
6
Hyperkeratosis:
Cause is chronic trauma.
Rarely pre-malignant.
Symptoms pain, pruritus, dyspareunia.
Signs white plaques.
Investigation biopsy.
Treatment care, removal of cause, steroid.
Dermatitis (eczema):
Types Contact dermatitis (only area of contact), allergic dermatitis (any area in the
body).
Causes of contact dermatitis soap, bubble path.
Causes of allergic dermatitis drugs, hair removal medication (sometimes lead to
contact dermatitis also).
Symptoms pain, redness, pruritus, dyspareunia.
Investigations skin test (patch test).
Treatment:
o Removal of affecting agent.
o Skin care (barrier).
o Antihistamine (alarmin).
o Iodine bicarbonate wash.
o Steroids.
Psoriasis:
Occur in flexion of body.
Features like psoriasis of other parts in the body.
Premalignant conditions:
Lichen sclerosis in elderly.
Human papilloma virus infection.
Valvar intra-epithelial neoplasm:
Vulval intraepitheial neoplasia (VIN) is a premalignant skin condition which is
increasing in incidence.

7
VIN can be either associated with human papilloma viruses (HPV) or with lichen
sclerosis.
Stages (dysplasia, one, two, three) like that of cervical cancer.
Presentation pain, pigmentation, pruritus, dyspareunia.
Investigations biopsy.
Treatment palliative therapy (laser cryotherapy), surgical removal and biopsy,
immunotherapy.
Do assessment of vagina and cervix.
Vulval cancer:
Vulval cancer is uncommon, with an incidence of ten cases per 100 000 women. There are
around 1000 newly diagnosed cases a year in the UK. These are skin tumours of the vulva
and are divided into HPVassociated (usually younger patients) and non-HPV (usually older
patients) cancers. The latter group may have their cancer associated with VIN and lichen
sclerosis.
Clinical presentation:
Vulval cancers usually present with vulval symptoms.
Patients may present with a lump (noticed when washing), vulval pain (some
tumours are ulcerating) and post-menopausal bleeding (some tumours bleed on
touch). Some patients are frequently unaware of vulval cancer.
While most tumours are small on examination, it is surprising how large some
tumours can be on initial presentation.
The tumours are usually clinically obvious and are often cauliflower-type growths on
the vulva.
Some tumours, however, can ulcerate and some may produce a subtle skin
thickening.
The most common sites are the labia majora and clitoris and the tumours may be
uni- or multifocal so it is important to examine the patient thoroughly (include the
anal area, vagina and cervix).
Vulval cancer spreads regionally to the groin nodes (inguinal and femoral) and
palpation of these nodes is important to exclude clinically obvious malignant nodes.
Patients should also have the cervix inspected to make sure that there is no
involvement by cancer or cervical intraepithelial neoplasia (CIN).
Pathophysiology:
Most vulval cancers are squamous cell cancers of the skin.
8
The lymphatic drainage of the vulva (and the lower third of the vagina) is to the
inguinal and femoral lymph nodes and this is the first place to which the tumour
metastasizes.
Beyond this, the tumour can spread up the lymphatic chain and finally to the liver
and lungs at a late stage.
Rarely vulval melanoma can develop and present with ulcerated and/or pigmented
lesions.
Treatment is by surgical excision of the primary site only.
Prognosis is poor and related to the depth of invasion.
Investigation and the importance of staging:
A biopsy is essential for diagnosis and a chest x-ray is useful to exclude obvious lung
metastases.
Staging of the cancer is essential for prognostic information and planning adjuvant
treatment.
Poor prognostic factors include large (greater than 4 cm) primary tumours, sphincter
involvement and metastases to the groin nodes.
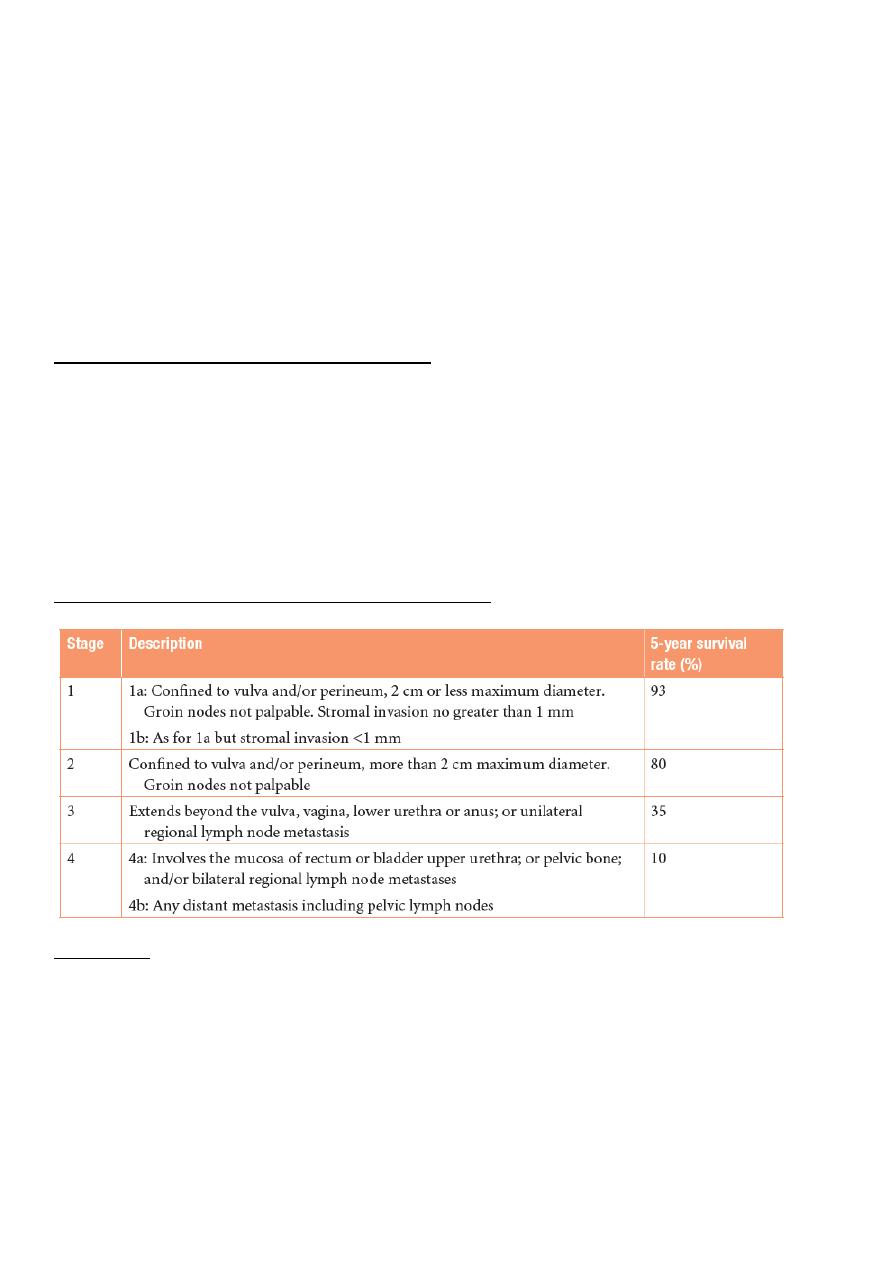
Staging and prognosis of vulval cancer (FIGO 2009):
Treatment:
Surgical radical vulvacetomy which include removal of vulva, blilateral L.N
(inguinal and femoral L.Ns).
Complication of surgery poor wound healing, wound breakdown, bleeding,
lymphedema, DVT, psychological and sexual problems.
Radiotherapy if L.N is involved.
Sentinel L.N if involved give radiotherapy, if not involved do surgery only.
Early stage tumor wide local excision.
9
Conditions that affect vagina:
Vaginal discharge:
Infection bacterial vaginosis, Trichomonas, candida.
Tumors of vagina, cervix, uterus.
Other F.B, trauma.
Lichen planus:
Involve vagina.
Give steroids suppositories and vaginal cream.
Lichen sclerosis: not involve the vagina.
Premalignant conditions:
Intraepithelial neoplasia can affect the genital tract (CIN and VIN).
Premalignant and malignant disease of the cervix.
The vaginal area can also be affected (called vaginal intraepithelial neoplasia, VAIN).
This is usually as a result of extension of CIN from the cervix.
VAIN is asymptomatic.
Treatment can involve cauterization, surgical excision, radiotherapy and
observational follow up depending on the patient, grade of disease and size of the
lesion.
VAIN assessment and treatment can be complicated and is best managed by
specialist teams.
There is a risk of vaginal cancer in untreated patients, but this risk remains unclear.
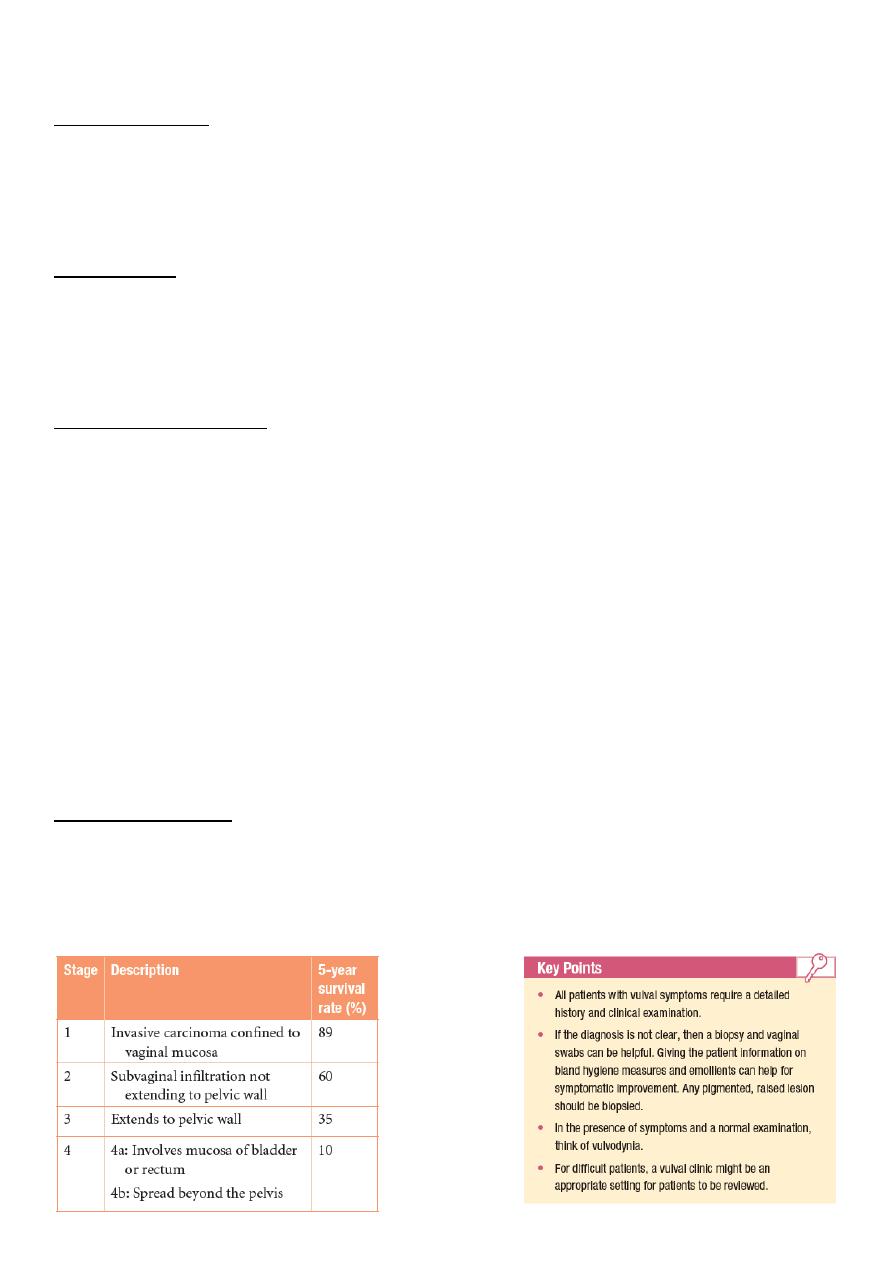
Malignant condition:
Will be missed so presented later and in metastatic state.
Treatment: radiation.
FIGO staging and prognosis of vaginal cancer:
