1
Fifth stage
Psychiatry
Lec-4
.د
صفية
10/3/2016
Conversion (dissociative) disorders
A loss or disturbance of normal motor or sensory function which initially appears to have
neurological or other physical cause but is later attributed to a psychological cause.
These disorders were initially explained by psychodynamic mechanisms---repression of
unacceptable conscious impulses and their ‘conversion’ to physical symptoms,
sometimes with symbolic meaning.
In ICD and DSM the presumed psychodynamic mechanisms are not part of the diagnosis.
Symptoms are not produced intentionally and the presence of secondary gain is not part
of the diagnosis.
2
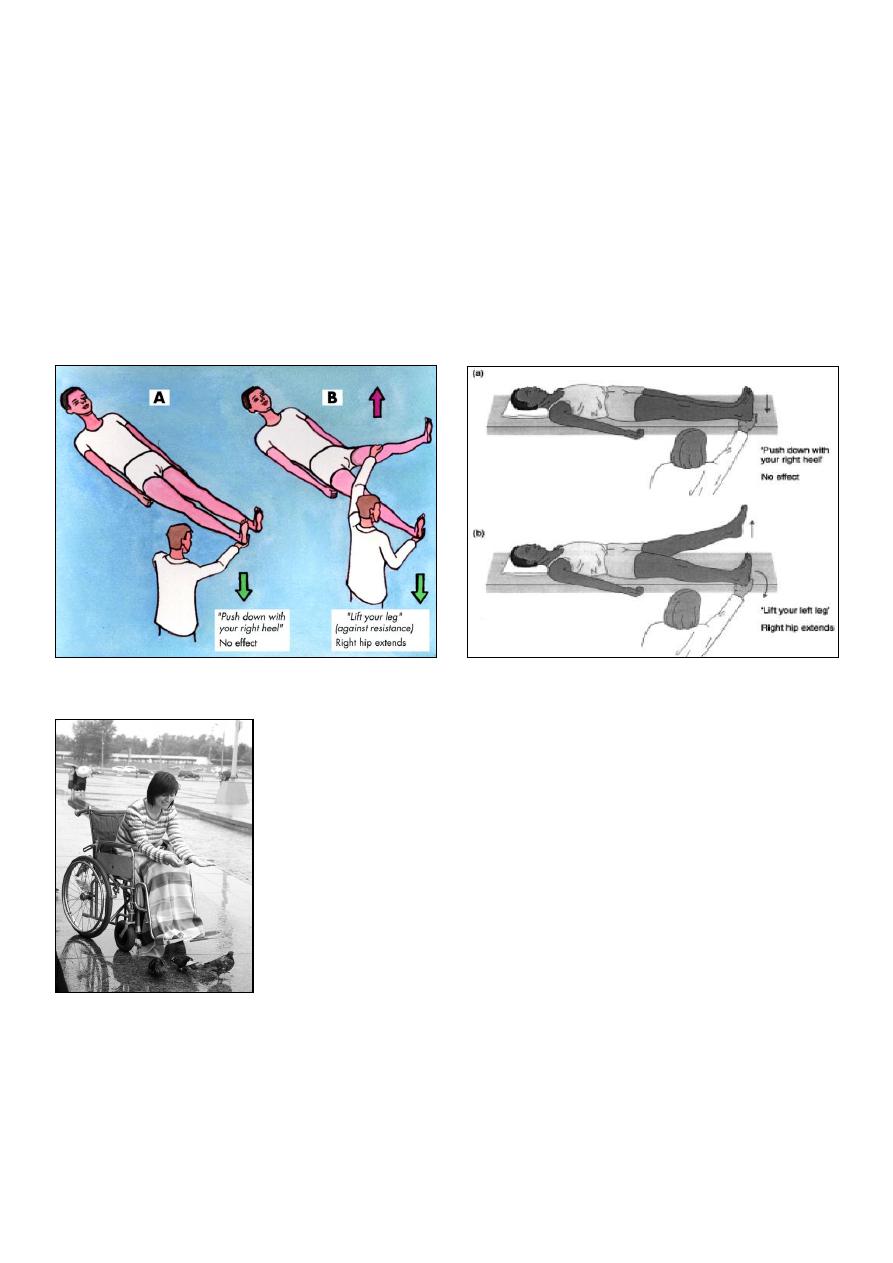
Paralysis:
One or more limbs or one side of the face or body may be affected.
Flaccid paralysis is common initially but severe, established cases may develop
contractures.
Often active movement of the limb is impossible during examination but synergistic
movement is observed (e.g. Hoover's test: the patient is unable to raise the affected limb
from the couch but is able to raise the unaffected limb against resistance with
demonstrable pressing down of the heel on the affected side).
Hoover’s test
la belle indifference
Loss of speech (aphonia)
There may be complete loss of speech, or loss of all but whispered speech.
There is no defect in comprehension and writing is unimpaired (and becomes the main
method of communication).
Laryngeal examination is normal and the patient's vocal cords can be fully opposed while
coughing.

3
Sensory loss
The area of loss will cover the patient's beliefs about anatomical structure rather than
reality (e.g. ‘glove’ distribution, marked midline splitting).
Seizures
Non-epileptic seizures are found most commonly in those with genuine epilepsy.
The non-epileptic attacks generally occur only in the presence of an audience,
no injury is sustained on falling to the ground,
tongue biting and incontinence are rare,
the seizure consists of generalized shaking, rather than regular clonic contractions, and
there is no post-ictal confusion or prolactin rise.
Amnesia
Memory loss,
most often for recent events,
not attributable to organic mental disorder, and
too severe to attribute to ordinary forgetfulness.
Usually patchy and selective amnesia (true global amnesia is rare).
There is expectation of recovery and usually a history of recent traumatic event gradually
emerges.
Fugue
Here there is dissociative amnesia plus a history of travel outside the patient’s normal
environs.
The patient may come to far from home, without memory of how they came to be there,
and
With variable amnesia for other personal information.
Although there is amnesia for the period of fugue, the patient has apparent functioned
normally during this time.
Recovery can be expected in time, and
a history of recent traumatic events is commonly found.
Diagnosis:
The diagnosis will usually be suspected due to the non-anatomical or clinically
inconsistent nature of the signs.
It is established by

4
1) excluding underlying organic disease, or demonstrating minor disorder insufficient to
account for the symptoms;
2) finding of positive signs (i.e. demonstration of function thought to be absent);
3) a convincing psychological explanation for the deficit.
Additionally helpful though non-specific is prior history of conversion symptoms or
recurrent somatic complaints or disorder
Family or individual stress and psychopathology (recent stress, grief, sexual abuse) or the
presence of a symptom model.
Treatment
Clear presentation of diagnosis in collaboration with treating medical team.
Aim to present the diagnosis as positive (emphasizing the likelihood of recovery) rather
than negative (we couldn’t find anything; it’s all in your head.
In general, avoid interventions which could maintain the sick role or prolong abnormal
function and instead consider interventions directed towards graceful resumption of
normal function (e.g. physiotherapy).
Treat psychiatric comorbidity if present.
CBT, IPT, supportive psychotherapy, family therapy, biofeedback are all potentially
helpful.
Prognosis
For acute conversion symptoms, especially those with a clear precipitant, the prognosis
is good, with expectation of complete resolution of symptoms (70-90% resolution at
follow-up).
Poorer outcomes for longer-lasting and well-established symptoms.
