
1
Fifth stage
ENT
Lec-13
د.سعد
14/3/2016
Tracheostomy
Tracheostomy is making an opening in the anterior wall of the trachea and converting it in to
a stoma on the skin surface.
Surgical anatomy
1- Trachea is situated normally in the midline but may be displaced to one side by an
enlarged thyroid gland or lymph node.
2- The trachea is more superficial at its upper end, it become deeper as it passes downward
so that at manuberum it is 1 inch from surface.
3- About 7-8 cartilaginous rings constitute the cervical portion of the trachea. Neck
extension draws more rings to the cervical portion.
4- In children: neck is shorter, larynx is higher and trachea is more superficial.
Function of tracheostomy
1- Alternative pathway for breathing.
2- Improve alveolar ventilation. In cases of respiratory insufficiency, alveolar ventilation is
improved by:
(a) Decreasing the dead space by 30-50% (normal dead space is 150 ml).
Dead space is
that is inhaled by the body in
, but does not take part in
gas exchange.
(b) Reducing the resistance to airflow.
3- Protects the airway: by using cuffed tube, tracheobronchial tree is protected against
aspiration of:
a- Pharyngeal secretions, as in case of bulbar paralysis or coma.
b- Blood in haemorrhage from pharynx, larynx or maxillofacial injuries.
4- Permits removal of tracheobronchial secretions. When patient is unable to cough in coma,
head injury, respiratory paralysis; or when cough is painful, as in chest injuries or upper
abdominal operations, the tracheobronchial airway can be kept clean of secretions by
repeated suction through the tracheostomy.
5- Intermittent positive pressure respiration (IPPR). If IPPR is required beyond 72 hours,
tracheostomy is superior to intubation.
6- To administer anaesthesia in cases where endotracheal intubation is difficult as in
laryngopharyngeal growths or trismus.
Types of tracheostomy
1. Elective temporary tracheostomy: This is performed as a planned procedure, usually
under GA, as a temporary stage in the patient's management (e.g. as a safety measure in
patient with head and neck surgery).
2
2. Permanent tracheostomy: This may be required in cases of bilateral abductor paralysis,
advanced laryngeal cancer or in laryngeal stenosis. In laryngectomy, the tracheal remnant
is brought out to the skin as a permanent mouth for respiratory tract.
3. Emergency tracheostomy: It is employed when airway obstruction is complete and there
is an urgent need to establish the airway. It is usually done under local anaesthesia.
Technique
The patient's neck is extended so the trachea comes immediately under the skin. Incision:
vertical incision is easier for beginner in the midline from the cricoid cartilage to suprasternal
notch. Then, separate the strap muscles of the neck. Thyroid isthmus is pushed up or down or
cut. A piece of tracheal cartilage is removed from 3
rd
and 4
th
tracheal rings and tracheostomy
tube is introduced.
Tracheostomy tubes:
1- The Silver Jackson tube: this is used for temporary tracheostomy and consists of outer
tube and inner tube which can be cleaned without disturbing the outer tube. It is inserted
over an introducer. It is metallic tube and its use is contraindicated during radiothyrapy.
2- Portex tube: both cuffed and uncuffed types. No introducers are used with them. There
is no inner tube, but they are almost non-irritant and safe during radiotherapy.
Post-operative care
1. Constant supervision, for bleeding, displacement or blocking of the tube and removal
of secretions.
2. Suction is required every half hour or so depending on amount of secretions.
3. Prevention of crusts and tracheitis, by proper humidification (e.g. by use of humidifier).
If crusting occurs, a few drops of normal saline are installed into the trachea every 2-3
hours to loosen crusts.
4. Care of tracheostomy tube. Inner cannula should be removed and cleaned when indicted
for the 1
st
three days. After 3-4 days the outer tube can be removed and changed every
day. On inserting the tube it is essential to check that it is in the trachea and not lying
anterior to it in the mediastinum. If this happens respiration will not be heard through
the tube and vascular erosion may occur.
If cuffed tube is used, it should be periodically deflated to prevent pressure necrosis or
dilatation of the trachea.
Complication of tracheostomy
1- Apnoea: this follows opening of trachea in a patient who had prolonged respiratory
obstruction. This is due to sudden washing out of CO2, which was acting as a
respiratory stimulus. Treatment is to administer 5% CO2+95% O2 or covering of
tracheostomy opening by plastic bag.
2- Subcutaneous surgical emphysema: due to escape of air around the tube. It may be
due to small tube or tight suturing of the wound. Air spread on the subcutaneous
3
plane to face, neck or arms. It is not dangerous unless it leads to mediastinal
emphysema. Treatment: open the skin widely and put appropriate size tube.
3- Blockage of the tube, due to lack of humidification or poor toilet. Treatment;
change the tube and remove the crusts by bronchoscopy.
4- Slipping of tube, where the tube lies in the cellular tissue in front of the trachea.
The patient has inspiratory stridor and speaks well without placing a finger on the
opening. It is due to small tube or low tracheostomy.
5- Failure of decannulation: overcome by progressive occlusion of the tube or use of
smaller and smaller tubes. Tube is blocked 24 hours before removal. If the patient
can sleep, eat and walk without dyspnoea then the tube can safely be removed.
6- Trachea-cutaneous fistula.
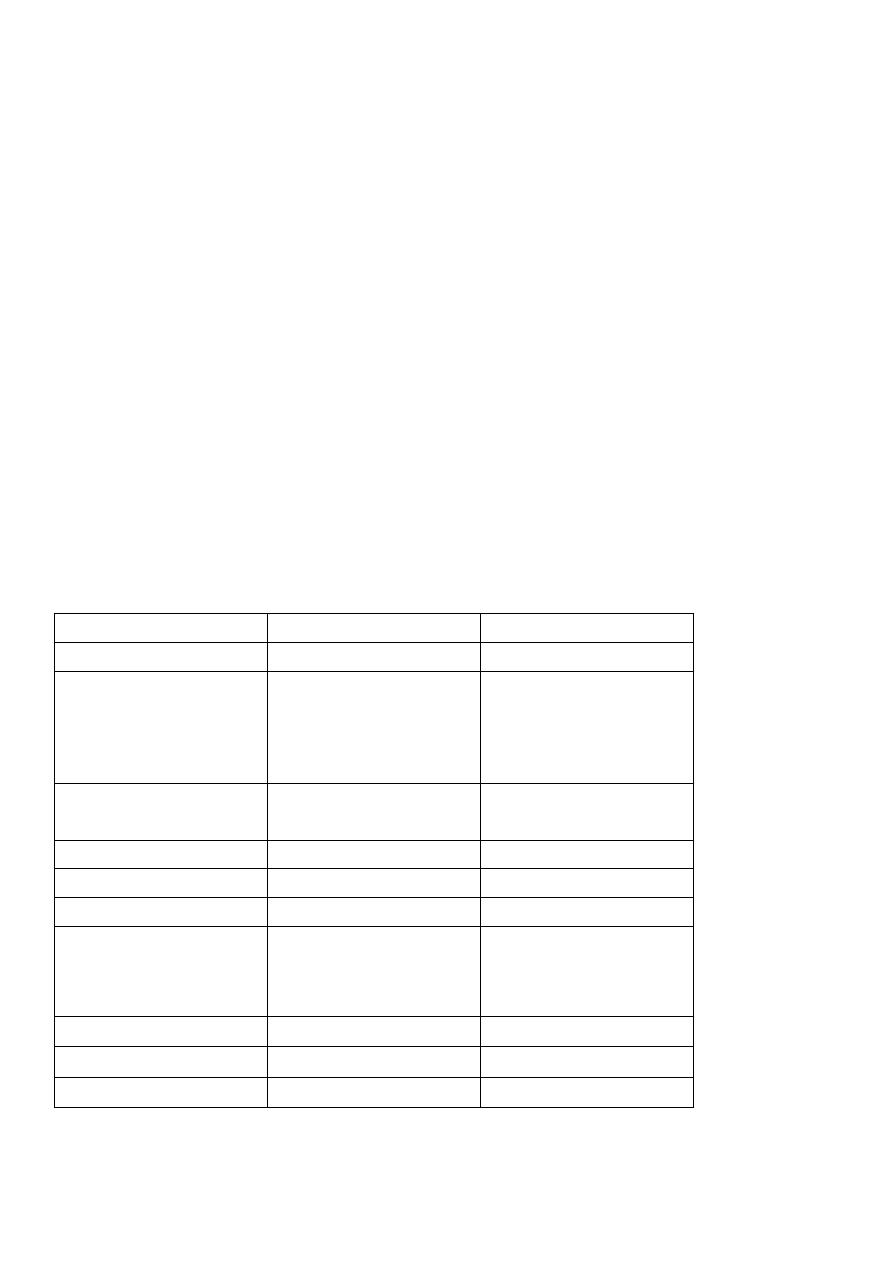
Intubation Versus Tracheostomy
Intubation is easier than tracheostomy, no anaesthesia, no wound and complications are
less. Tracheostomy is more difficult and takes longer time. In any patient who needs
intubation for more than 3 days, tracheostomy must be done for him. (See the table
below)
Intubation versus Tracheostomy
Intubation
Tracheostomy
Time
Quick procedure
Takes longer time
Nursing
Needs
specialized
I.C.U due to the risk
of obstruction and
dislodgement.
Less
specialized
facilities
Talking
and
coughing
Impossible
Possible by closing
the tube
Feeding
By NGT
Normal
Sedation
Necessary
Not necessary
Complications
a- Pneumothorax
and
surgical
emphysema
Negative
Positive
b- Scar
Negative
Positive
c- Dislodgement
Dangerous
Less dangerous
d- Obstruction
Common
Less common
