
1
Fifth stage
Gynecology
Lec-1
.د
و
لدان
16/3/2016
Infertility
Objectives of this lecture:
1. To define infertility.
2. To know the prevalence and types of infertility.
3. To know the requirement of normal fertility.
4. To know the causes of infertility.
Defintion:
Infertility is defined as the inability to conceive after one year of unprotected vaginal
intercourse and without contraception and in the absence of pathological conditions.
Prevalence: 15-20% of couples.
It could be:
• Primary infertility: the couples never achieved pregnancy.
• Secondary infertility: the couples have previous successful pregnancy even if ended
by abortion.
Requirements for normal fertility:
• Ovulation and spermatogenesis.
• Patent tubes, normal cervix and uterus, normal vas and urethra (pathways).
• Normal male sexual function.
• Normal cervical mucus secretion.
Infertility is not a disease, it is a symptom that something is preventing the reproductive
processes from working properly, and needs treating.

2
Causes of infertility:
• Male factor – 23 percent.
• Ovulatory dysfunction – 18 percent.
• Tubal damage – 14 percent.
• Endometriosis – 9 percent.
• Coital problems – 5 percent.
• Cervical factor – 3 percent.
• Unexplained – 28 percent.
Factors affecting fertility:
1. Age: female fertility is highest in the late teens and early twenties. In male fertility
started at puberty and continue throughout life but declines after 60 y.
2. Health and nutrition: weight loss affect fertility, obesity is associated with infertility.
3. Psychological factor: anxiety and stress.
Female infertility:
I.
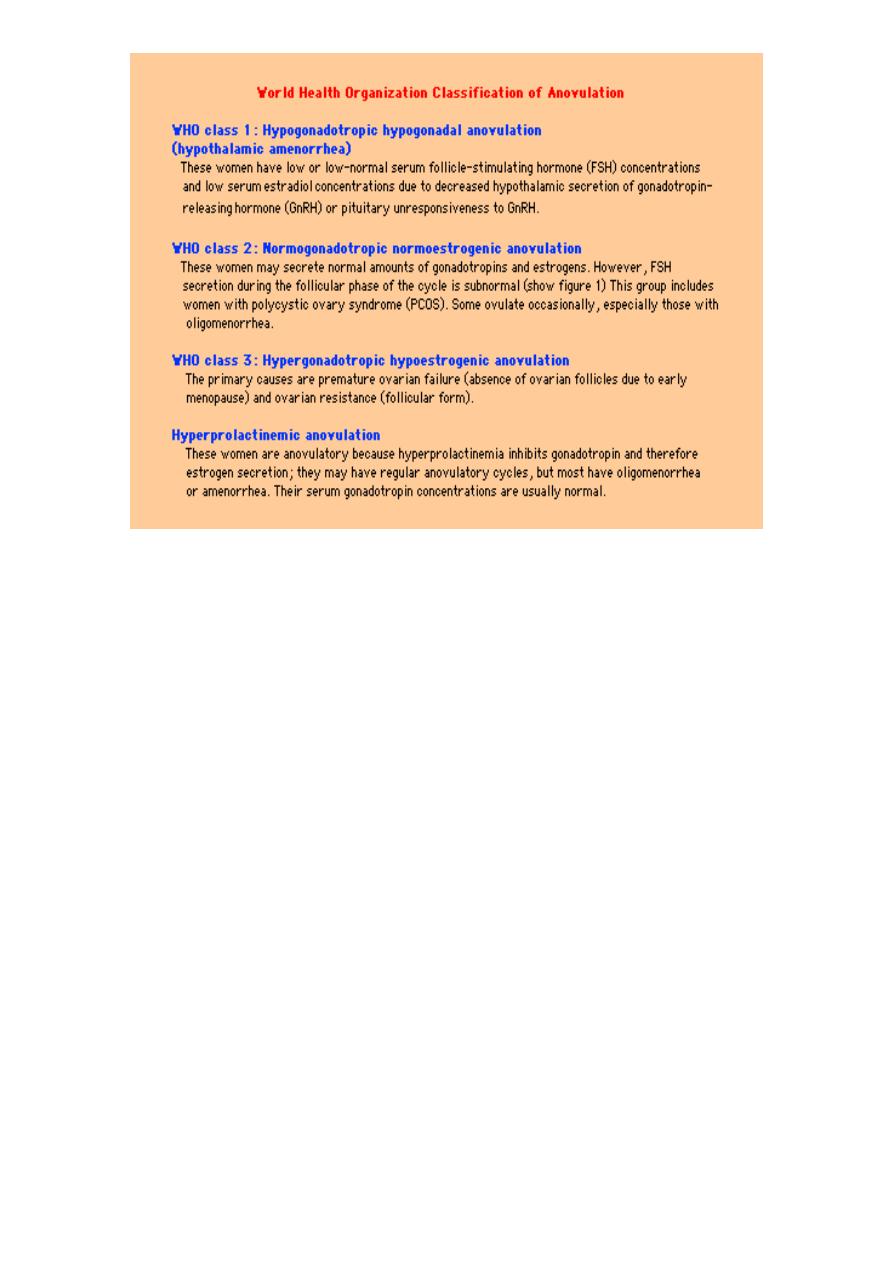
Ovulatory failure:
A. Endocrine causes:
• hypothalamus: stress, drugs, altered body mass.
• Pituitary: macro and micro adenoma secreting prolactin.
• Thyroid disease.
• Adrenal disease.
B. Primary ovarian dysfunction:
• Resistant ovary syndrome.
• PCOS.
• Absent ovaries and absent oocytes.
3
II. Failure of oocyte or embryo transport:
A. Tubal block from:
1. Salpingitis.
2. Tubal sterilization.
3. Endometriosis.
4. Pressure from outside like big uterine fibroid.
B. Endometrial cavity obliteration by
1. Big uterine fibroid.
2. Intrauterine adhesions (Ashermans syndrome).
C. Cervical mucus hostility: caused by:
• No ovulation ( no estrogen).
• Infections.
• Antisperm antibodies.

4
Evaluation of an infertile couple:
The factors that should be evaluated and the relevant tests that should be performed
include the following:
• Male factor – semen analysis: Semen analysis can be performed at any time during the
menstrual cycle, preferably collected on site after 48 to 72 hours of abstinence.
• Ovulatory function – endometrial biopsy or serum progesterone.
• Cervical factor – postcoital test.
• Uterine factor – hysteron salpingography and/or hysteroscopy, pelvic ultrasonography.
• Tubal factor – hysteron salpingography and laparoscopy.
• Endometriosis or other pelvic pathology – laparoscopy.
The standard semen analysis consists of the following:
• Measurement of semen volume and Ph.
• Microscopy for debris and agglutination.
• Assessment of sperm concentration, motility, and morphology.
• Sperm leukocyte count.
• Search for immature germ cells.
Semen volume – The normal semen volume is 2 to 5 mL.
Sperm concentration – Sperm concentration, is normally above 20 million/mL.
Sperm motility – At least 60 percent of spermatozoa should be motile.
Sperm morphology – At least 70% normal.
Postcoital test
The postcoital test provides information on the interaction between sperm and cervical
mucus. It is performed one to three days before ovulation, and involves taking a sample of
cervical mucus two to twelve hours after coitus. The cervical mucus should show ferning
and >5 cm spinnbarkeit (defined as the distance a mucus thread can be pulled before
breaking) At least five motile sperm per high power field should be seen.

5
Assessment of ovulation
A clinical assessment of ovulation can be made from the menstrual history:
• Amenorrhea signifies the absence of ovulation and certainly represents a cause of
infertility.
• Oligomenorrhea implies irregular menses and erratic ovulation.
• Regular, predictable cyclic menses almost always reflect regular ovulation, and probably
also assure normal serum concentrations of the hormones commonly ordered in infertility
evaluations, including follicle-stimulating hormone (FSH), luteinizing hormone (LH),
prolactin, and androgens.
• A basal-body-temperature chart may be used to confirm the clinical impression of
ovulation. There will be a biphasic curve during an ovulatory cycle, with temperatures in the
luteal phase higher by 0.5 to 1.0°F due to progesterone production by the corpus luteum.
• Urinary LH surge testing.
• Definitive confirmation of ovulation can be obtained by measurement of serum
progesterone in the mid-luteal phase, 18 to 24 days after the onset of menses. Normal mid-
luteal phase serum progesterone concentrations usually vary from 6 to 25 ng/mL (19 to 80
nmol/L).
• Endometrial biopsy in the luteal phase.
Role of hysteron salpingography and laparoscopy –
The former should be included as a standard component of the initial evaluation, because it
can often eliminate the need for laparoscopy. Hystero salpingography should be performed
during the period between the cessation of menses and ovulation.
If a cause is found and no conception occurs after a specified number of cycles (e.g six), then
laparoscopy might be warranted.
