
1
Fifth stage
Surgery
Lec-4
.د
أركان
29/3/2016
Regional anesthesia
• Regional anaesthesia is ideal for many operations, in particular those on the limbs
and lower abdomen
• For many other operations regional analgesia can complement general anaesthesia
and provide lasting and effective postoperative pain relief.
• preoperative assessment and preparation as for general anaesthesia
- full explanation of the procedure, and consent.
- preparation of drugs and equipment for general anaesthesia and resuscitation, in addition
to those required for the regional technique chosen.
Advantages of regional anaesthesia:
◗ conscious patient, able to assist in positioning, and warn of adverse effects (e.g. in carotid
endarterectomy and TURP).
• There is less interruption of oral intake, especially beneficial in diabetes mellitus.
◗ good postoperative analgesia.
◗ reduction of certain postoperative complications, e.g. atelectasis and DVT, possibly
myocardial ischaemia
Contraindications:
◗ absolute: patient refusal, localised infection.
◗ relative: abnormal anatomy or deformity, coagulation disorders, previous failure of the
technique, and neurological disease or other medicolegal considerations
Local anesthetic drugs: -
1. Amide linked local anesthetic drugs; lignocaine, prilocaine, bupivacaine.
2. Ester linked local anesthetic drugs; cocaine , benzocaine , amethocaine

2
Commonly used local anaesthetics Drugs
• Lidocaine
Medium-acting amide. Maximum safe dose 4mg/kg without adrenaline, 7mg/kg with
adrenaline .
• Prilocaine
Medium-acting amide. Used for intravenous regional anaesthesia due to its rapid
metabolism. Maximum safe dose 6mg/kg without adrenalin, 8mg/kg with adrenaline
• Bupivacaine
Long-acting amide. Maximum safe dose 2mg/kg with or without adrenaline.
• Amethocaine
Long-acting ester. Rapid absorption from mucous membranes or transdermal route.
• Benzocaine
Short-acting ester. Used as lozenges
• Cocaine
Short-acting ester. Slow onset, profound vasoconstriction by preventing noradrenaline
reuptake.
Adrenaline: -
Added to local anaesthetic solution to: -
1. Decrease blood flow at the site of injection, leading to decrease vascular absorption &
increase neuronal uptake of local anaesthetic, so the depth & duration of neuronal
blockade are increased.
2. Decrease the likelihood of high blood level local anaesthetic (decrease toxic reaction to
local anaesthetic).
3. In infiltration technique, local vasoconstriction leads to decrease bleeding.
3
Side effects:
• If injected intravenously may cause cardiac effect ventricular tachycardia VT,
ventricular fibrillation VF, hypertension, and myocardial ischemia.
• Should not be used for ring block of digit, penis, tip of nose that may cause
vasoconstriction of end arteries & lead to ischemia & gangrene.
The clinical manifestations of local anesthetic toxicity
CNS toxicity
• Light-headedness, tinnitus, perioral numbness, confusion
• Muscle twitching, auditory and visual hallucinations
• Tonic-clonic seizure, unconsciousness, respiratory arrest
Cardiotoxicity
• Hypertension, tachycardia
• Decreased contractility and cardiac output, hypotension
• Sinus bradycardia, ventricular dysrhythmias, circulatory arrest
Topical anaesthesia: -
Most local anaesthetics produce rapid anaesthesia when applied to mucous membranes.
Sites: eye (conjunctiva), nasal cavity, throat, larynx, ear, urethra.
Application: instillation, spray, ointment, pastes, gels.
1. EMLA cream: mixture of lignocaine & prilocaine for application to the skin
before venipuncture, this is especially valuable for children but take one hour
to act.
2. Lignocaine: 4% maximum 5ml in 70kg man.
3. Cocaine: 5% maximum 5ml in 70kg man.
Nerve blocks: neck
• Superficial cervical plexus block
• Deep cervical plexus block
Nerve blocks: upper limb
4
• Interscalene brachial plexus block
• Supraclavicular block
• Vertical infraclavicular block
• Coracoid block
• Axillary block
• Mid-humeral block
• Elbow block
• Wrist block
• Digital block
• Intravenous regional anaesthesia–Bier’s block
Nerve blocks: trunk
• Thoracic paravertebral block
• Intercostal nerve block
• Inguinal field block
• Penile block
Nerve blocks: lower limb
• Lumbar plexus block
• Femoral nerve block
• Lateral cutaneous nerve of the thigh block
• Sciatic nerve block
• Popliteal sciatic nerve block
• Saphenous nerve block
• Ankle block
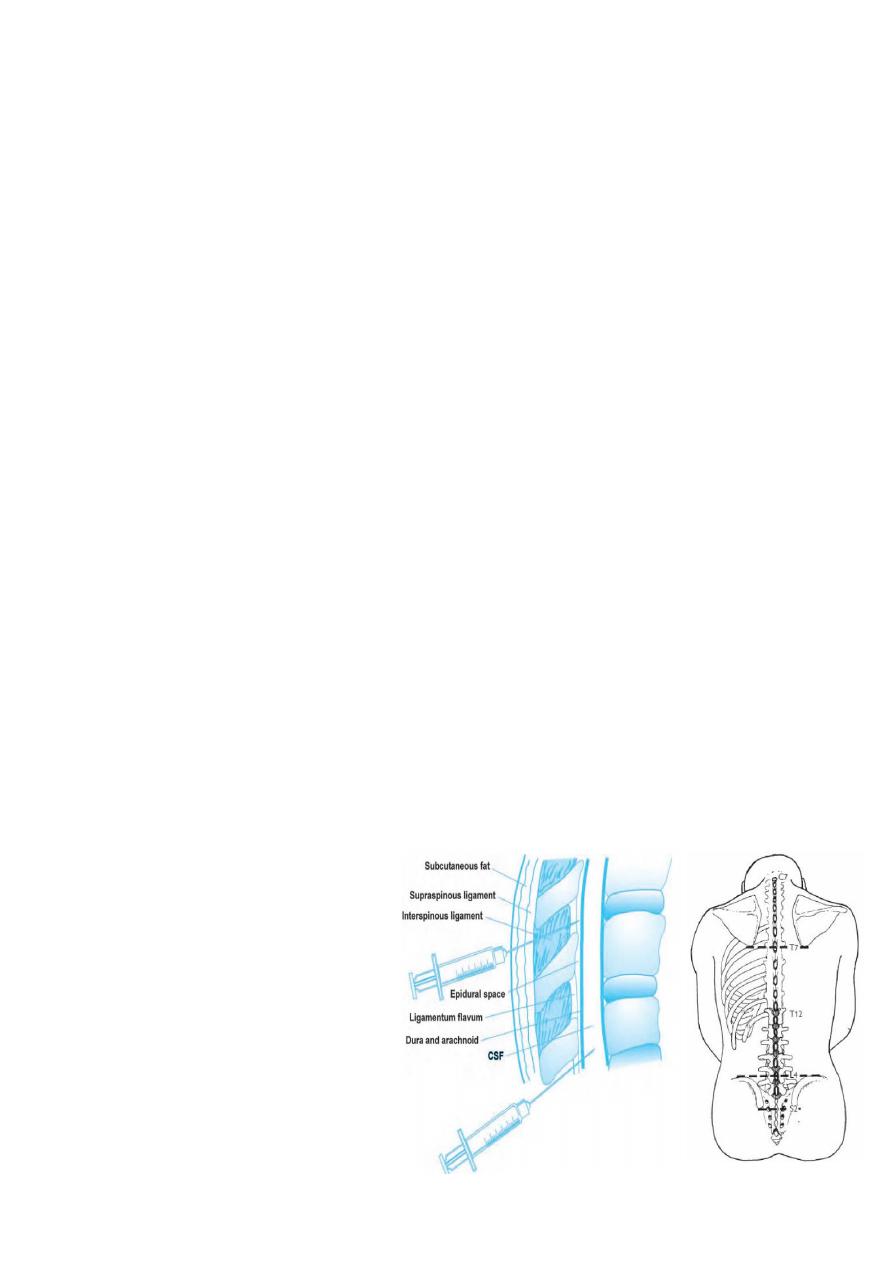
Nerve blocks: neuraxial
• Spinal and epidural
