1
Fifth stage
ENT
Lec-17
د.سعد
4/4/2016
Acute Otitis Media (AOM)
Definition; is an acute inflammation of the lining of the middle ear cleft. It is extremely
common in children but can occur at any age. There is nearly always a preceding history of
URTI.
Sources of infection
1- Through the ET following URTI.
2- Through the EAM if there is a pre-existing perforation of the TM.
3- Blood borne infection.
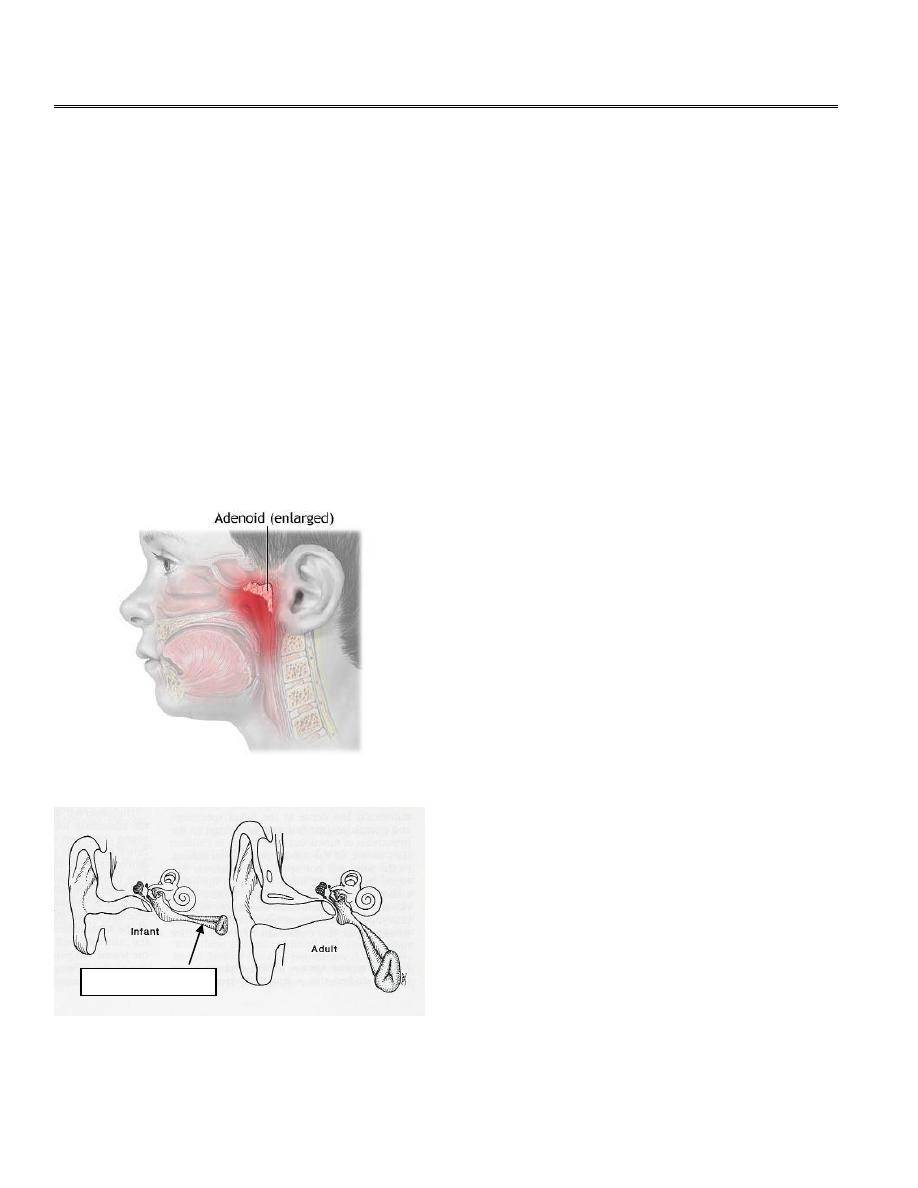
Age
Acute otitis media is distinctly more common
in infants and children than in adults. This is
due to:
1. Hypertrophy of adenoids
2. More frequent URTI (the child has
poorly developed immunity to URTI)
3. Less effective ET function because it
is shorter, wider and more horizontal
and opens at a lower level in infant’s
nasopharynx.
4. Teething (lowers resistance)
5. Inability to blow the nose
6. Bottle feeding facilitates acute otitis
media by:
• Recumbent position of the child
• Milk is less sterile
Eustachian tube
2
Bacteriology
There is initial viral infection which paves the way for pyogenic infection. The commonest bacteria
isolated are Pneumococci, H. influenzae, and Branhamella catarrhalis, a beta lactamase producing organism.
Pathology
The process usually started by URTI leading to infection of the ET (salpingitis). The air within the middle is
absorbed and replaced by exudates which may later become purulent. This suppuration if not treated leads
to rupture of the TM and relief of pain.
Clinical Picture
The onset is fairly sudden and commonly there is a preceding URTI:
1. Pain (earache) is the most prominent symptom and usually it is described as sharp
lancinate in character.
2. Conductive hearing loss due to fluid accumulation in the middle ear.
3. Mucopurulent discharge indicates rupture of the TM and usually associated with pain
relief.
4. Constitutional symptoms as pyrexia, malaise, vomiting and diarrhea.
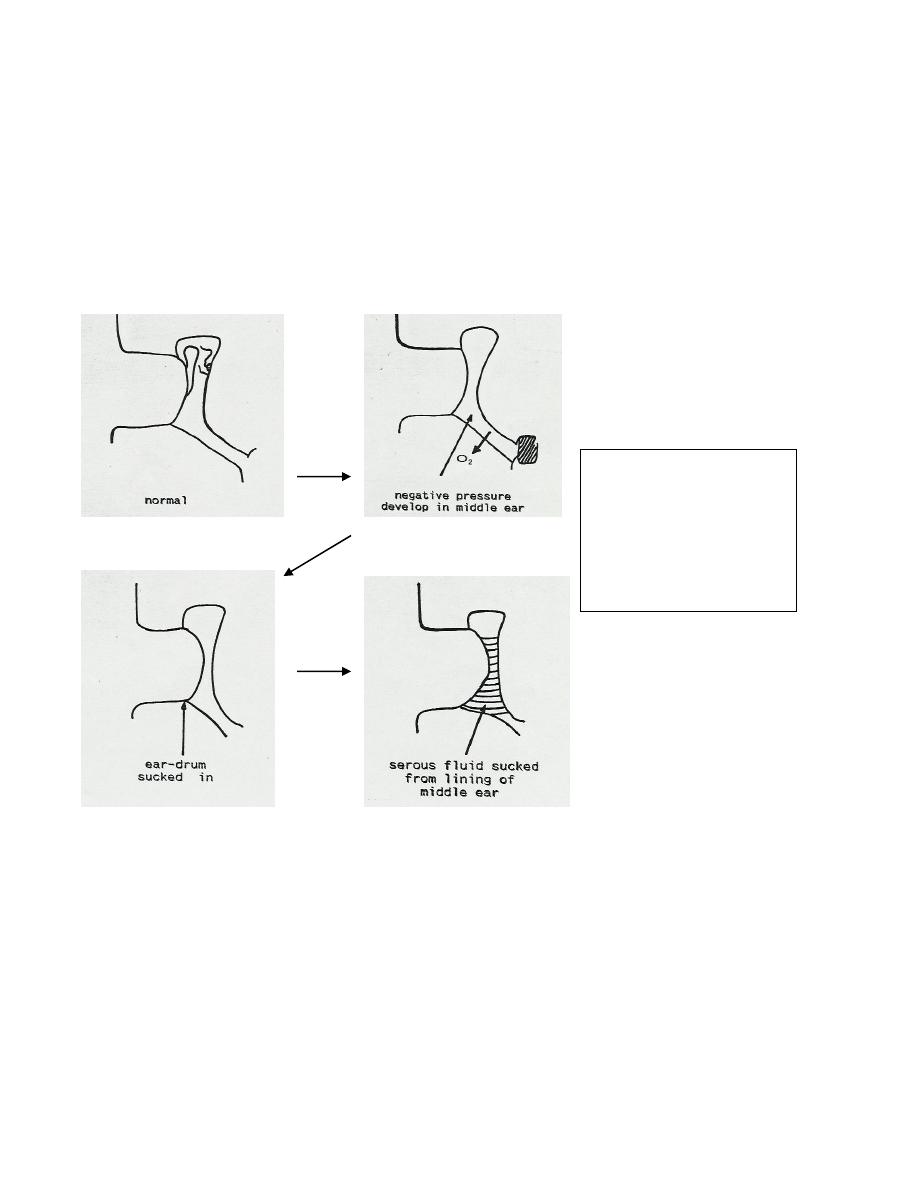
The figures show the
mechanism for development
of fluid inside the middle ear
in case of AOM and
secretory otitis media-see
below.

3
Examination
1. Otoscopy: Redness and injection of the TM and in severe cases there is outwards
bulging of the TM. A mucopurulent discharge filling the EAM can be seen if
perforation of the TM has occurred.
2. Examination of the nose and oropharynx
3. Tuning fork test: Conductive hearing loss; Rinne test is negative and Weber test is
lateralized to the affected ear.
4. P.T.A.: Conductive hearing loss.
Treatment
Medical:
1. Treatment of URTI.
2. Bed rest, heat application and Analgesics e.g. aspirin or paracetamol.
3. Decongestant nose drops: Ephedrine hydrochloride (0.5-1%) or nasophrine.
4. Antibiotics: given for 7-10 days as follow;
Amoxycillin or Amoxycillin-clavulanic acid combination for beta- lactamase-
producing organisms
, constitutes the first choice.
If patients sensitive to penicillin,
Erythromycin or Co-trimoxazole or cefixime
may be used.
5.
AOM with discharge ( Acute suppurative otitis media);
-
Dry mopping by wisps of cotton wool.
-
Prevent water from entering the ear.
-
Swab should be taken for culture and sensitivity.
-
Antibiotic-steroid drops may be used in those patients in whom the discharge
remains.
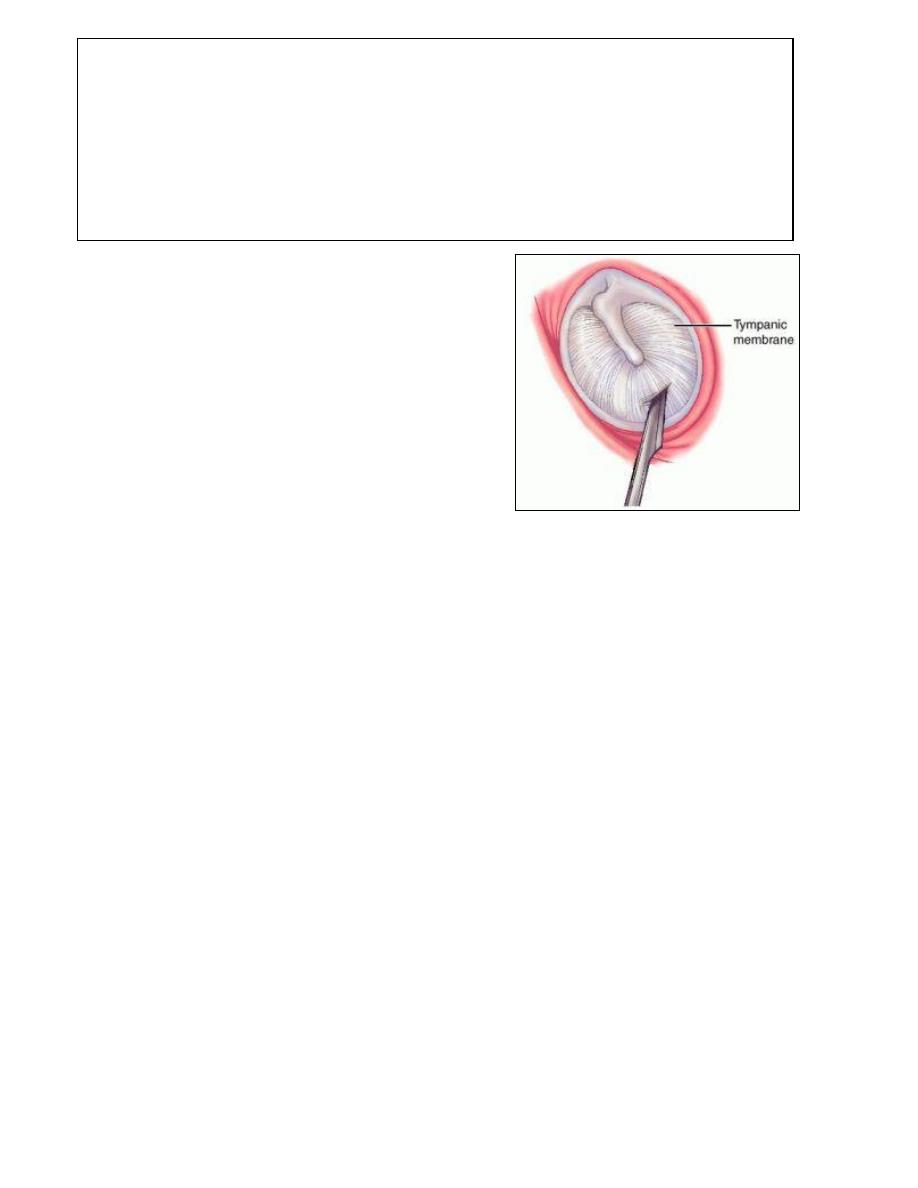
Surgical
Myringotomy is indicated if there is
severe pain not responding to treatment. A
swab for bacteriological study is mandatory
and continuing antibiotic therapy will
depend upon the result. The object of
myringotomy is not only pain relief but to
facilitate healing with a good firm surgical
scar instead of risking a large perforation
closed with a thin fragile membrane.
4
Prognosis of ASOM (Acute suppurative otitis media )
1. Healing: the perforation may be closed with a scar that is invisible.
2. Open perforation either dry or moist with deafness.
3. Tympanosclerosis: white chalk-like patches on the surface of the TM produced
by calcium deposition.
4. Adhesive OM: formation of adhesion which bind the TM to the medial wall of the
middle ear. They may also adhere to the ossicles causing CHL.
5
Chronic Middle Ear Disease
1. Non-suppurative: Secretory otitis media or otitis media with effusion.
2. Suppurative: Chronic suppurative otitis media (CSOM).
3. Tuberculous.
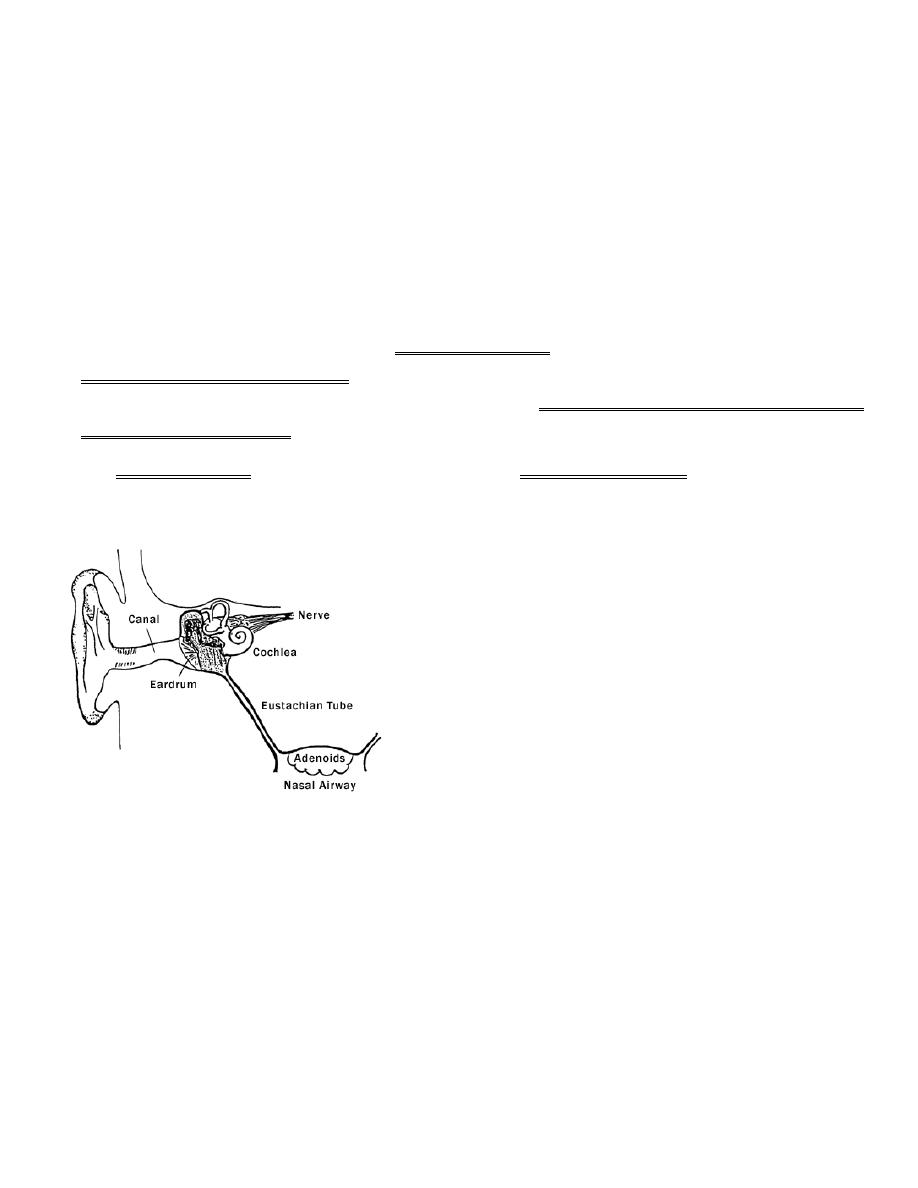
Otitis Media with Effusion
(OME, Glue ear or Secretory otitis media)
Definition; Accumulation of fluid (non-purulent fluid) in the middle ear, occurring in the
absence of acute inflammation. It may vary from thin serous fluid to thick viscid material.
This is a very common condition and undoubtedly the most frequent cause of acquired
hearing loss in childhood.
It is usually bilateral but may be unilateral, and it is usually intermittent.
Aetiology
1. Occlusion of Eustachian tube which
may result from:
a) Adenoid hypertrophy.
b) Tubal infection (salpingitis) due to
extension of infection from URT but
not progressing to ASOM.
c) Traumatic stricture or adhesion
following adenoidectomy.
d) Postnasal mass: antrochoanal polyp
or nasopharyngeal CA.
2. Unresolved acute otitis media either from failure of natural immunity or inadequate
antibiotic therapy.
3. Nasal allergy.
4. Barotrauma; descent in an airplane or diving.
5. Cleft palate.
6
Pathophysiology: (see the fig. in page 2)
There is an initial ET obstruction due to various causes resulting in air absorption from the
middle ear and vacuum formation. Consequently, the TM drawn inwards followed by
transudation of 'sterile' secretion from the mucous membrane to fill the middle ear. This fluid
accumulation leads to CHL and with time this thin fluid changes to thick glue one.
Clinical picture:
The condition is suspected in children suffering from repeated tonsillitis with adenoid
hypertrophy and in adult when CHL follow influenza or common cold.
1. Insidious conducive hearing loss: it is the commonest cause of hearing loss in
childhood between 4-6 years of age. Changes in head position causes changes in
degree of deafness when the fluid is thin.
2. Tinnitus: Crackling, bubbling noises and sensation of fluid in the ear.
3. Pain occurs only if acute infection supervenes.
Examination
1. Otoscopy:
a) The TM is dull, retracted and often has a yellow orange tint.
b) Dilated blood vessels running parallel to the handle of malleus (cart-wheel
appearance).
c) Air bubbles or a fluid level may be seen when the fluid is serous.
2. Siegle`s pneumatic speculum: The tympanic membrane lacks of normal mobility
3. Tuning fork test: negative Rinne test .Weber is lateralized to the affected ear.
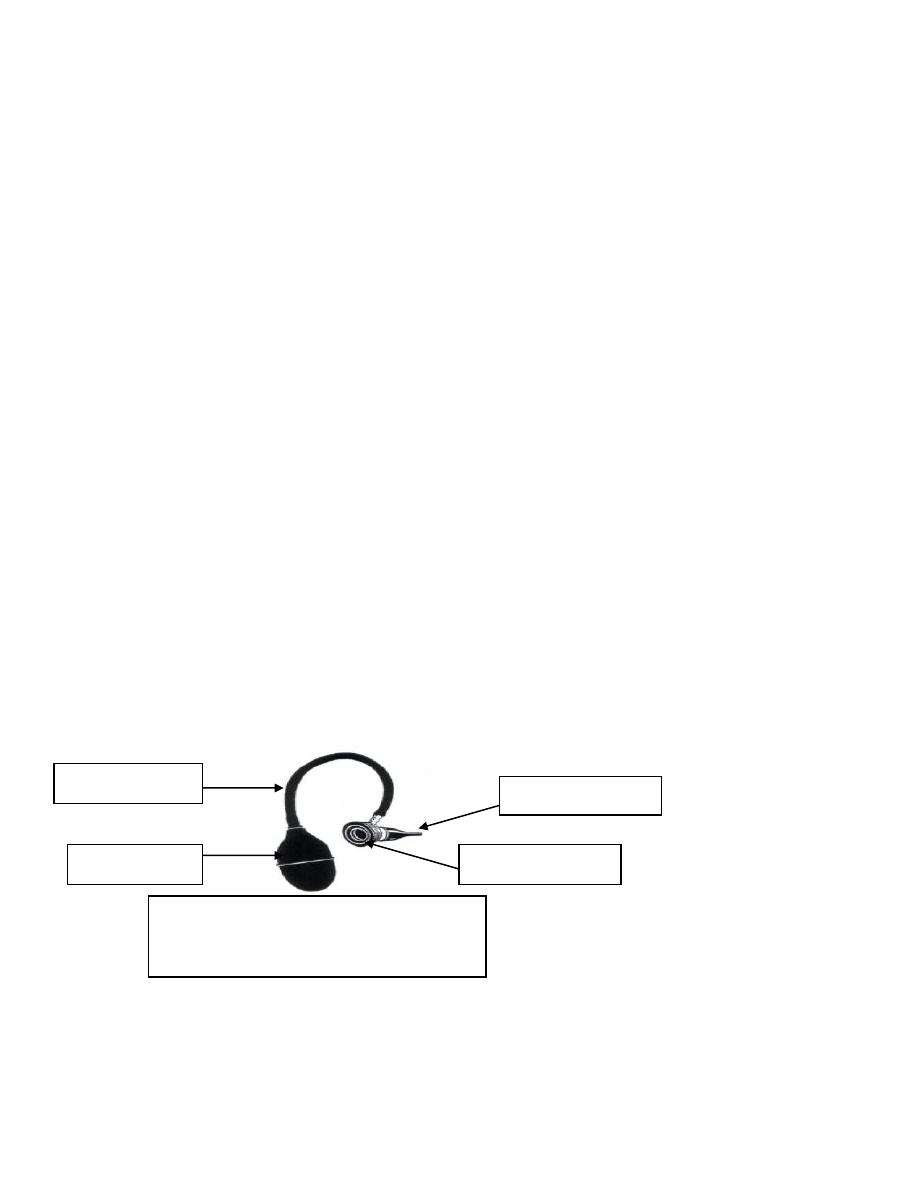
Aural speculum
Magnifying lens
Rubber tube
Rubber ball
The figure shows the parts of Siegle`s
pneumatic speculum which is used for
checking the integrity and mobility of TM
7
Investigation
a) PTA: CHL of at least 40 dB.
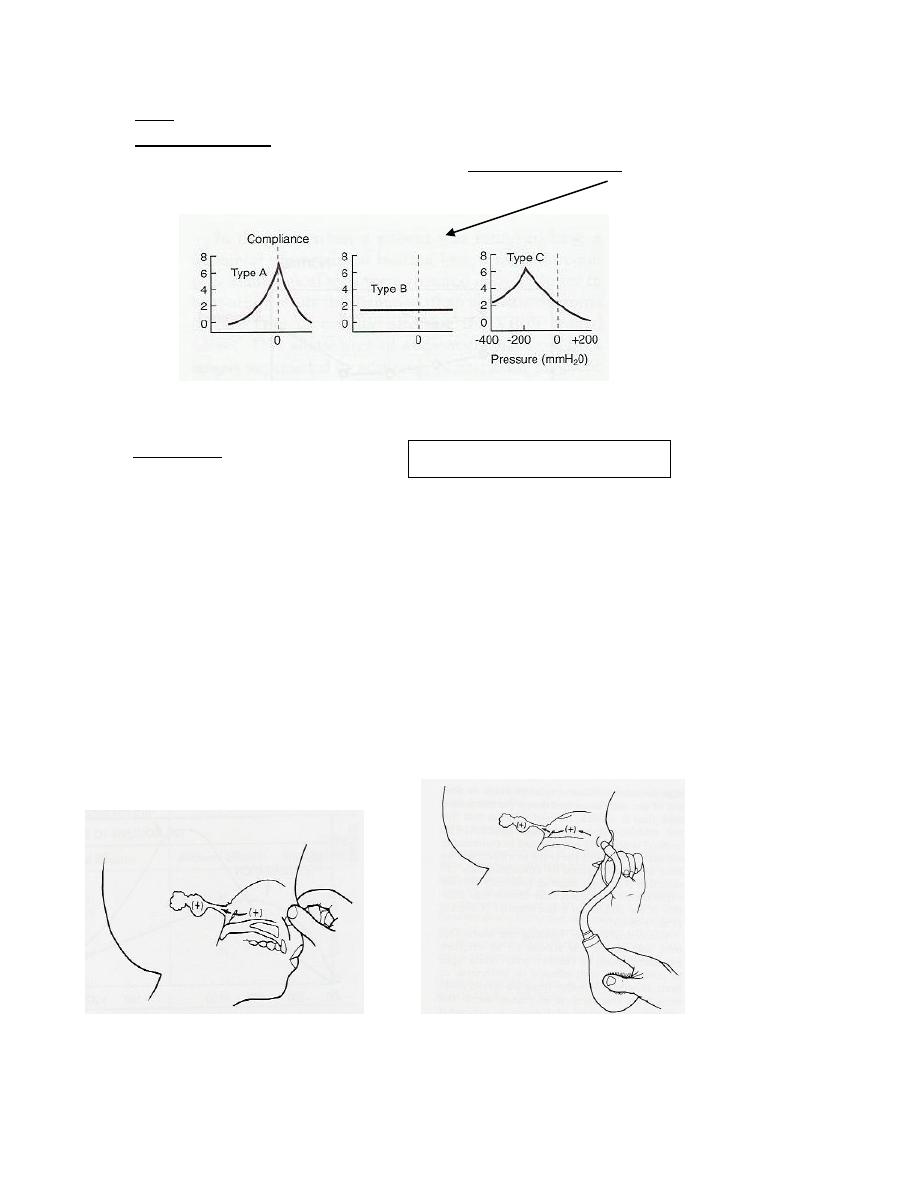
b) Tympanometry: a special device used to measure the compliance and resistance (i.e.
impedance) of middle ear, will show a flat tympanogram
c) Radiology: sinus X-ray and views of the post nasal space to exclude adenoid
hypertrophy and space occupying lesion.
Treatment
1. Treatment of the predisposing factors
: e.g. adenoidectomy, treatment of nasal and sinus
infection and closure of cleft palate.
2. Medical
a) Decongestant nose drops.
b) Antihistamines in patients with allergic rhinitis.
c) Mucolytic agents e.g. solvodin.
d) Steroid nasal spray
e) Antibiotics: Long-term low dose antibiotics may be beneficial in 50% of cases.
f) Repeated auto-inflation (Valsalva Maneuver and Politzerization)
Valsalva maneuver Politzerization
CHL= Conductive Hearing Loss
8
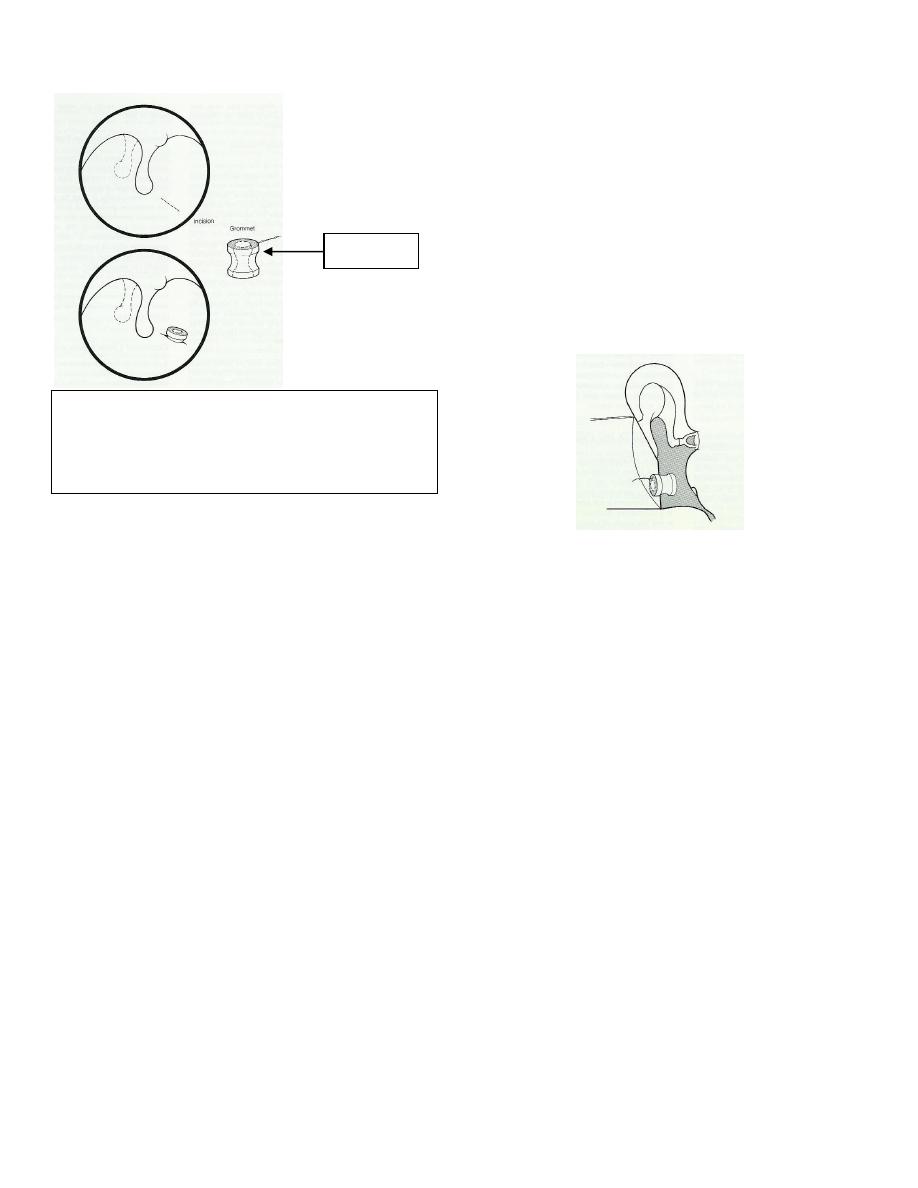
3. Surgical
Surgery should only be recommended for
diseases persistent more than 3 months. The
surgical treatment consists of myringotomy,
aspiration of thick mucoid material and the
insertion of grommet. This grommet
provides adequate ventilation of the middle
ear and is essentially an artificial ET. After
several months however, the grommet is
slowly extruded.
Grommet
Complications of OME
1. Retraction pockets and
cholesteatoma.
2. Tympanosclerosis.
3. Adhesive otitis media.
