
1
Fifth stage
Dermatology
Lec-9
.د
عمر
10/4/2016
Atopic Dermatitis
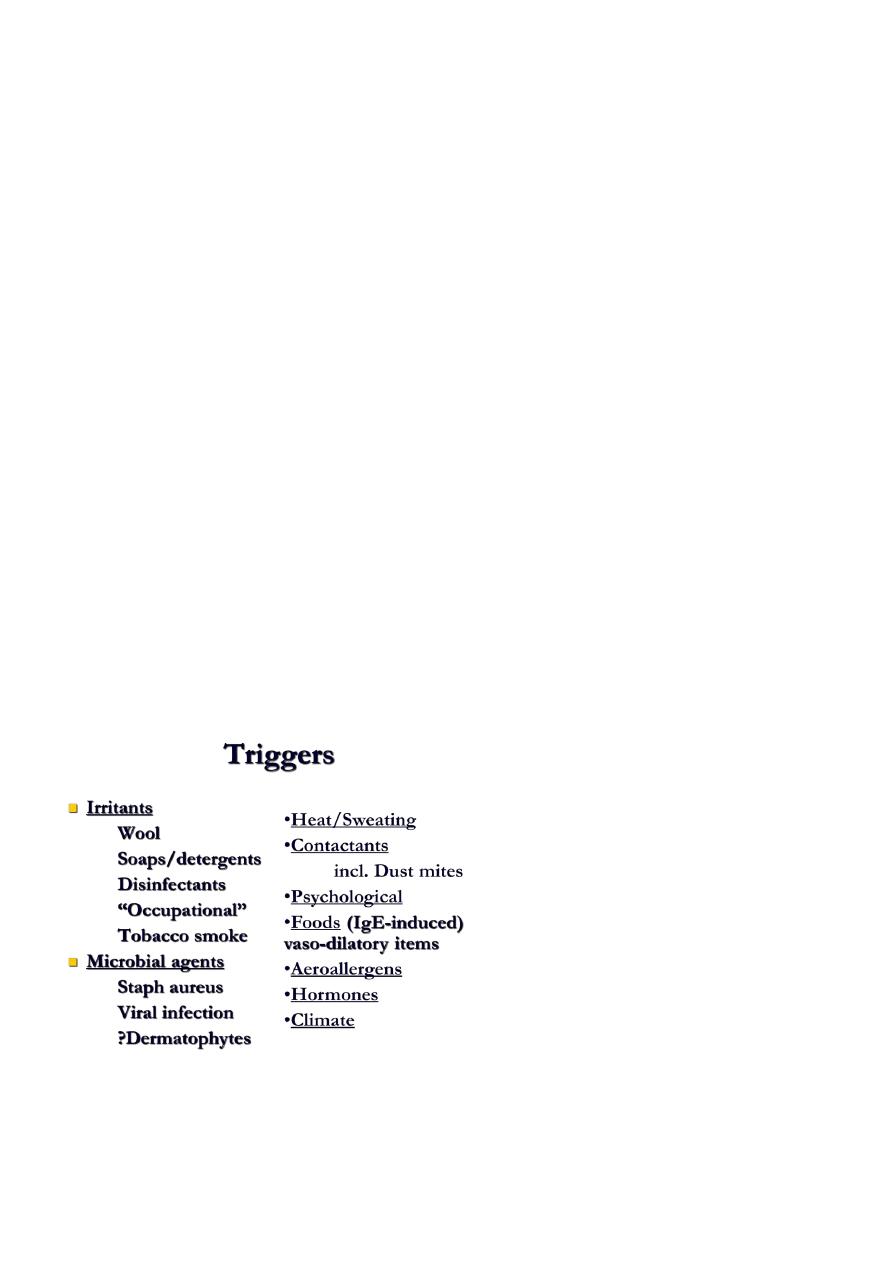
Atopic dermatitis (AD) is a chronic, highly pruritic, eczematous skin disease that follows
patients from early childhood into puberty and sometimes adulthood.
Also referred to as eczematous dermatitis, the disease often has a remitting/flaring
course, which may be exacerbated by social, environmental, and biological triggers.
Prevalence
Approximately 15% in the US and Europe
This represents a profound increase in recent years (from as low as 3% in 1960)
Natural History of Atopic Dermatitis
60% of pts develop AD by 1 year of age.
85% of pts develop AD by age 5.
Earlier onset often indicates a more severe course.
Many cases resolve by age 2, improvement by puberty is common.
50%-60% of pts develop respiratory allergies or asthma.
80% of occupational skin disease occur in atopics.
It is rare to see AD after age 50.
Filaggrin
Filaggrins are filament-associated proteins which bind to keratin fibers in epithelial cells
Individuals with truncation mutations in the gene coding for filaggrin are strongly
predisposed to a severe form of dry skin, ichthyosis vulgaris, and/or eczema
It has been shown that almost 50% of all severe cases of eczema may have at least one
mutated filaggrin gene.
2
Infantile atopic dermatitis
Infants less than one year old often have widely distributed eczema. The skin is often
dry, scaly and red with small scratch marks made by sharp baby nails.
The cheeks of infants are often the first place to be affected by eczema +- head +-
body.
The diaper area is frequently spared due to the moisture retention of diapers. Just like
other babies, they can develop irritant diaper dermatitis, if wet or soiled diapers are
left on too long.
3
Toddlers and pre-schoolers
As children begin to move around, the eczema becomes more localized and thickened.
Toddlers scratch vigorously and the eczema may look very raw and uncomfortable.
Eczema in this age group often affects the extensor (outer) aspects of joints,
particularly the wrists, elbows, ankles and knees. It may also affect the genitals.
As the child becomes older the pattern frequently changes to involve the flexor
surfaces of the same joints (the creases) with less extensor involvement. The affected
skin often becomes lichenified i.e. dry and thickened from constant scratching and
rubbing,
In some children the extensor pattern of eczema persists into later childhood.
Atopic dermatitis in school-age children
Older children tend to have the flexural pattern of eczema and it most often affects the
elbow and knee creases. Other susceptible areas include the eyelids, earlobes, neck
and scalp.
Many children develop a 'nummular' pattern of atopic dermatitis. This refers to small
coin-like areas of eczema scattered over the body. These round patches of eczema are
dry, red and itchy and may be mistaken for ringworm (a fungal infection).
Mostly the eczema improves during school years and it may completely clear up by the
teens, although the barrier function of the skin is never entirely normal.

4
Managing AD (Preventative)
Prevent “scratching” or rubbing
a) apply cold compresses to itchy skin
Carefully eliminate all the triggers of itch
a) environmental, occupational, and temperature control
b) bathing – soapless cleansers, Dove
c) LUBRICATION – LUBRICATION - LUBRICATION
Managing AD (Palliation)
Topical anti-inflammatory agents
a) corticosteroids (ointments>creams)
more potent - when “acute”
least potent needed for “chronic”
b) Tacrolimus 0.1%, 0.03% ointment
Pimecrolimus 1% Cream
Emollients
Atopic dermatitis patients frequently have dry skin which is aggravated during winter
months.
Xerosis (dryness) breaks the barrier function of the skin and promotes infection and
inflammation.
Ointments are preferred over lotions or creams.
Emollients should be applied immediately after a soaking bath to retain the moisture.
Emollients containing urea or alpha-hydroxy acids often cause stinging or burning
sensations.
Corticosteroids
These are the cornerstones of therapy of atopic dermatitis. The following principles
should be adhered to while instituting topical steroid therapy:

5
High potency steroids are used for a short period to rapidly reduce inflammation.
Maintenance therapy, if needed is best done with mild steroids like hydrocortisone.
On face and intertriginous areas, mild steroids should be used, mid-potency
formulations are used for trunk and limbs.
Topical steroids are applied initially twice or three times a day. After the symptoms are
lessened, frequency of application should be reduced. Intermittent use if topical
steroid may be alternated with application of emollients.
Ointments are superior to creams or lotions.
The potential side-effects of topical steroids should always be kept in mind.
Systemic steroids: a short course of systemic steroids (prednisolone, triamcinolone)
may occasionally be needed to suppress acute flare-ups.
Intralesional steroids (triamcinolone acetonide) may help resolve thickened plaques of
eczema not responding to topical agents
Calcineuron Inhibitors
Indications
Protopic (tacrolimus) Ointment, both 0.03% and 0.1% for adults; 0.03% for children
aged 2-15 years
o For short-term and intermittent long-term therapy in the treatment of
moderate to severe atopic dermatitis in patients
For whom the use of alternative, conventional therapies are deemed
inadvisable because of potential risks
or
Who are not adequately responsive to, or are intolerant of alternative,
conventional therapies.
Elidel (Pimecrolimus Cream 1%) for patients 2 years of age and older
o For short-term and intermittent long-term therapy in the treatment of mild to
moderate atopic dermatitis in non-immunocompromised patients
For whom the use of alternative, conventional therapies are deemed
inadvisable because of potential risks
or
Who are not adequately responsive to, or are intolerant of alternative,
conventional therapies.

6
Antihistamines
Antihistamines give variable results in controlling pruritus of atopic dermatitis since
histamine is not the only mediator of itching in atopic patients.
Any of the non-sedating antihistamines like cetirizine, loratadine or fexofenadine may
be used.
The conventional antihistamines like diphenhydramine or hydroxyzine may give better
results for their additional actions as a sedative or anxiolytic.
Topical antihistamines should be avoided for their sensitizing potential (Doxepin
cream).
Oral immunomodulators
Cyclosporine:
By virtue of its immunomodulating action, cyclosporine has a limited role in controlling
atopic dermatitis in recalcitrant adult cases. The potential side effects should always be
kept in mind.
Azathioprine:
This immunosuppressive agent has also been used in severe adult cases. Again, potential
side effects limit its role in selected cases.
Complications of AD
Secondary Infection
a) bacterial
impetiginization
“super-antigenicity”
b) viral
Localized – verruca, molluscum, herpes
Generaized – Dermatitis herpetiformis
c) mycotic
Dermatophyte
Candidal
