
1
Fifth stage
Dermatology
Lec-10
.د
عمر
10/4/2016
Hair Disorders
Types of Hair
• There are three types of hair. Thick, pigmented hairs are called terminal hairs.
Terminal hairs on the top of the head and in the beard, axillary, and pubic areas are
influenced by androgens. Androgens are important in regulating hair growth (at
puberty).
• Lanugo hairs are the fine hairs found on the fetus; similar fine hairs (peach fuzz)
found on the adult are called vellus hairs.
• Vellus hair is short, fine, and relatively nonpigmented and covers much of the body.
Hair on the rest of the body is independent of androgens.
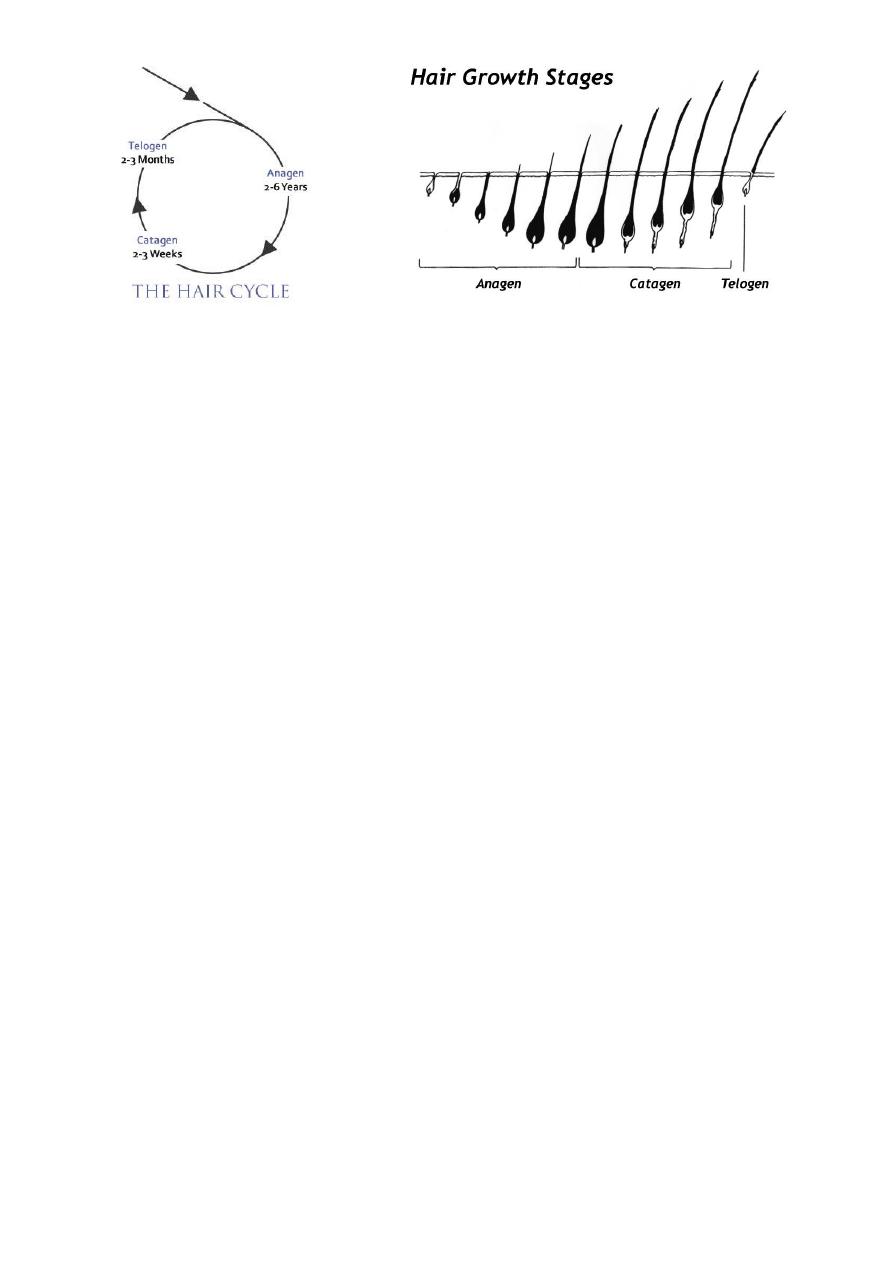
Hair growth cycle
• The average scalp has more than 100,000 hairs.
• The anagen (growth) phase of scalp hair is approximately 1000 days (range, 2 to 6
years).
• Hair in other area has a shorter growth phase.
• Scalp hair grows 0.3 to 0.4 mm/day, or approximately 6 inches a year.
• Approximately 90% to 95% of hairs are in the anagen phase.
• The duration of anagen determines the length of hair.
• Less than 1% of scalp hairs are in the catagen (involution or death) phase in which
the follicular keratinocytes die.
• About 5% to 10% are in the telogen (resting) phase which lasts 2-3 months before
the scalp follicles renter the anagen and the cycle is repeated.
• Up to 100 telogen hairs are lost each day from the head, and about the same number
of follicles enter anagen.
2
Hair Loss
Telogen effluvium
GENERALIZED
TELOGEN EFFLUVIUM
Acute blood loss
Childbirth
Crash diets (inadequate protein)
Drugs
Coumarin
Heparin
Propranolol
Vitamin A
High fever
Hypothyroidism and hyperthyroidisms
Physical stress (e.g., surgery)
Physiologic (e.g., neonate)
Psychologic stress
Severe illness (e.g., systemic lupus erythematosis)
• A number of events have been documented that prematurely terminate anagen and
cause an abnormally high number of normal hairs to enter the resting, or telogen,
phase.
• The follicle is not diseased but has had its biologic clock reset and undergoes a
normal involutional process.

3
• Usually no more than 50% of the patient’s hair is affected.
• Scarring and inflammation are absent.
• Resting hairs on the scalp are retained for approximately 100 days before they are
lost; therefore telogen hair loss should occur approximately 3 months after the event
that terminated normal hair growth.
• Sudden diffuse loss of club hairs 2 to 3 months later.
• Hair loss begins abruptly and lasts for approximately 4 weeks (full recovery can be
expected without treatment).
Androgenetic Alopecia in Men (Male Pattern Baldness)
• Baldness in men is not a disease, but rather a physiologic reaction induced by
androgens in genetically predisposed men.
• The pattern of inheritance is probably polygenic.
• Thinning of the hair begins between the ages of 12 and 40 years, and about half the
population expresses this trait before the age of 50.
Pthophysiology
• Androgenetic alopecia is due to the progressive shortening of successive anagen
cycles.
• There are two populations of scalp follicles: androgen-sensitive follicles on the top
and androgen-independent follicles on the sides and back of the scalp.

4
• In genetically predisposed individuals, and under the influence of androgens,
predisposed follicles are gradually miniaturized, and large, pigmented hairs (terminal
hairs) are replaced by thin, depigmented hairs (vellus hairs).
• Inflammation surrounds the bulge area of the outer root sheath. The inflammation
may damage the follicle stem cells, which results in a decrease in hair-follicle density.
• Hair follicles are still present, but removing androgens or treatment with minoxidil or
finasteride does not result in the conversion of miniaturized follicles back to terminal
ones.
Finasteride
• Finasteride (Propecia 1 mg) taken daily is an effective oral therapy for androgenetic
alopecia in men.
• In men with male pattern hair loss, finasteride 1 mg/day slowed the progression of
hair loss and increased hair growth in clinical trials over 2 years. Therapy leads to
slowing of further hair loss.
• Efficacy is evident within 3 months of therapy. The drug produces progressive
increases in hair counts at 6 and 12 months.
Treatment
Minoxidil
• Minoxidil was developed to treat hypertension. It increases the duration of anagen,
causes follicles at rest to grow, and enlarges miniaturized follicles.
• One milliliter of solution is applied twice daily to dry scalpand spread lightly with a
finger.
• Spontaneous reversal to the pretreatment state occurs in 1 to 3 months after
stopping treatment.
• Ideal candidates are men younger than 30 years of age who have been losing hair for
less than 5 years.
• The solutions produce a modest increase in hair on scalps of young men and women
(with with mild to moderate hair loss, with continuous twice daily application for
years to maintain the effect.
• Dizziness and tachycardia have been reported with 2% solution. Local irritation,
itching, dryness, and erythema may occur.

5
Alopecia Areata
• Alopecia areata (AA) is a common asymptomatic disease characterized by the rapid
onset of total hair loss in a sharply defined, usually round, area.
• The diagnosis is made by observation. Any hair-bearing surface may be affected. The
cause is unknown.
• An interaction between genetic and environmental factors may trigger the disease.
• Alopecia areata is a partial loss of scalp hair, alopecia totalis is 100% loss of scalp hair,
and alopecia universalis is 100% loss of hair on the scalp and body
Prevalence
• The incidence of AA in the United States is 0.1% to 0.2% of the population.
• Sixty percent of patients present with their first patch before 20 years of age.
• Familial incidence is 37% in patients who had their first patch by 30 years of age and
7.1% in patients who had their first patch after 30 years of age.
Clinical Presentation.
• Most patients report the sudden occurrence of one to several 1- to 4-cm areas of hair
loss on the scalp that can be easily concealed by covering with adjacent hair.
• The skin is smooth and white or may have short stubs of hair.
• The hair shaft in AA is poorly formed and breaks on reaching the surface.
• Some patients complain of itching, tenderness, or a burning sensation before the
patches appear.
• AA progresses as a wave of follicles prematurely enters telogen.
• The event weakens or narrows the hair shaft, which continues to grow before the
telogen phase is complete.
• Most weakened hairs fracture when they reach the surface.
• The affected hairs that are often found retained at the periphery of a lesion have a
normal upper shaft and a narrowed base—”exclamation point” hair.
• Regrowth begins in 1 to 3 months and may be followed by loss in the same or other
areas.

6
• The new hair is usually of the same color and texture, but it may be fine and white.
Occasionally the white color remains.
• The eyelashes, beard, and, rarely, other parts of the body may be involved.
• Total hair loss of the scalp (alopecia totalis), seen most frequently in young people,
may be accompanied by cycles of growth and loss, but the prognosis for long-term
regrowth is poor.
• Total body hair loss (alopecia universalis) is very rare.
Nail Changes.
• Nail dystrophy may be associated with AA. The incidence is 10% to 66%.
• Pitting with an irregular pattern, or in organized transverse or longitudinal rows and
longitudinal striations, may result in a sandpaper appearance seen in one or all of the
nails of some patients with AA.
• Dystrophy precedes, coincides with, or occurs after resolution of AA.
Prognosis
• The course is unpredictable; recovery may be complete or partial.
• Several episodes of loss and regrowth are typical. The prognosis for total permanent
regrowth in cases with limited involvement is excellent.
• Most patients entirely regrow hair within 1 year without treatment; 10% develop
chronic disease and may never regrow hair.
• Patients with a family history of AA, young age at onset, immune diseases, nail
dystrophy, atopy, and extensive hair loss have a poor prognosis.
Treatment
• Intralesional steroids
• Topical steroids
• Systemic setroids
• Minoidil
• Minoxidil plus topical stroid
• Anthralin

7
• Topical immunotherapy
• Cyclosporin
• Wigs
Primary Scarring Alopecia (Classification based on Clinical Presentation and Histology)
Initially lymphocytic
• Chronic cutaneous lupus erythematosus
• Lichen planopilaris
• Classic lichen planopilaris
• Frontal fibrosing alopecia
• Lassueur-Graham-Little syndrome (LPP and LP and spinous lesions)
• Pseudopelade (Brocq)
• Central centrifugal cicatricial alopecia (follicular degeneration syndrome, hotcomb
alopecia)
Neutrophilic
• Folliculitis decalvans
• Dissecting cellulitis/folliculitis
Mixed
• Acne keloid
• Tufted folliculitis
• Acne necrotica
• Erosive pustular dermatosis
