بسم الله الرحمن الرحيم
Femoral shaft fracture
This fracture occurs at any age, it is common especially in young adults, and usually results from a high energy injury, such as
( car accident , fall from height).
In elderly ,
it may be pathological fractureIn children think of child abuse.
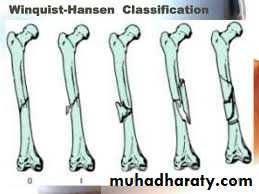
Fracture may be
spiral,transverse, comminuted, pathological,
or compound.
Most fractures have some degrees of comminuation (small fragment, single large butter fly, extensive comminuation).
Clinically:
The patient has pain and swelling,the leg externally rotated, short, deformed, swollen, bruises.
Always try to exclude neurovascular injury,
and look for possible serious life threatening injuries.
The fracture result in a significant
blood loss of 0.5-1.5 liter , shock and fat embolism are common early complications.
X-ray :
Shows the type of fractures, and displacement. The x-ray should include the hip and knee and x-ray of pelvis to avoid missing segmental fractures, knee injuries, fractures of neck of femur, dislocation of hip, fractures of acetabulum and pelvis.
.
Emergency treatment :
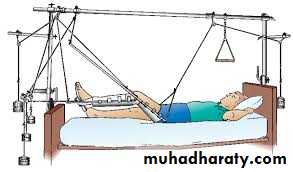
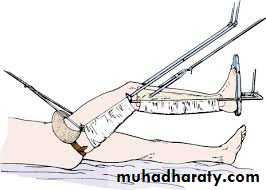
Traction with a splint (Thomas’ splint) is first aid for a patient with a femoral shaft fracture, Shock treatment, and early transport to hospital.Thomas splint
Open fractures treated by debridement and external fixation.
Definitive treatment
closed fractures: by Open reduction and internal fixation, this will decrease the systemic complications..
Fixation of femoral shaft fracture
Exercises for the lower leg and foot are important in preserving muscle tone and in preventing deformity and they should be begin immediately
Conservative treatment:
Reduction and holding by traction,( fixed traction, balanced traction with or without splint followed by exercise) rarely applied.
COMPLICATIONS
Early complications:1- Shock & blood loss (1-2 litres lost even in closed fractures)
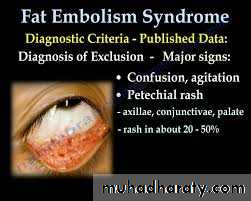
2- Fat embolism and acute respiratory distress syndrome ( formation of fat globules in blood or showering of fatty emboli from the marrow to the lungs)
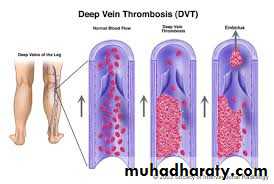
3- Deep vein thrombosis and pulmonary embolism ( specially with prolonged traction in bed).
4- Infection (in open fractures) and skin damage.
Late complications:
1- Delayed union
and
non-union need rigid fixation and bone graft .
2- Malunion (Fractures treated by traction and bracing often develop some deformity; no more than 15 degrees of angulations or rotation should be accepted)
3- Joint stiffness (specially knee joint, may be injured at the same time or adhesions during treatment)
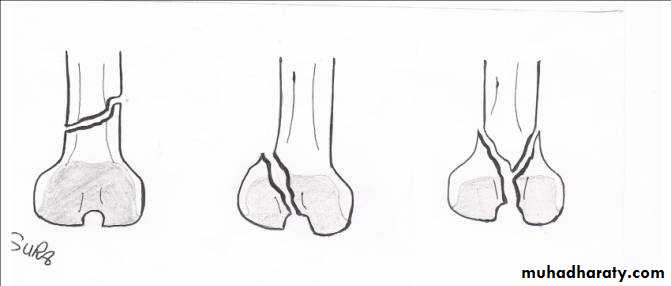
Supracondylar fractures of the femur
Typically the fracture occurs just proximally to the point where the medial and lateral cortices of the femur flare out to form condyles. In young it follow sever trauma and in old follow osteoporosis.A vertical extension of the fracture may split the two condyles apart in a T – shaped fracture line, and sometime there is more extensive comminuation.
Clinically :
pain and deformity in lower thigh after trauma.Knee is swollen and distal pulses should be palpated.
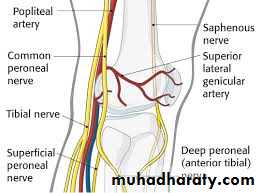
It may injured the popliteal artery and nerves.
pain and deformity in lower thigh after trauma.
Knee is swollen and distal pulses should be palpated.It may injured the popliteal artery and nerves.
Treatment :
These fractures can sometimes be treated successfully by traction through the upper tibia in young, followed by cast brace.
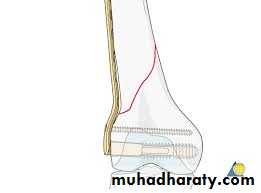
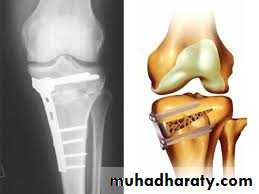
In old internal fixation is often preferable and the patient can get out of bed sooner (dynamic condylar screw and plate) .
dynamic condylar screw and plate
Supracondylar fracture with its fixation by L – plate and screwsComplications
popliteal vessels injuries.nerve injury (common peroneal nerve).
Malunion.
delayed union .
and stiffness of knee.
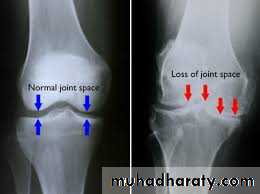
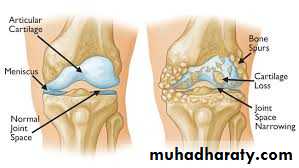
Deformities of the knee joint
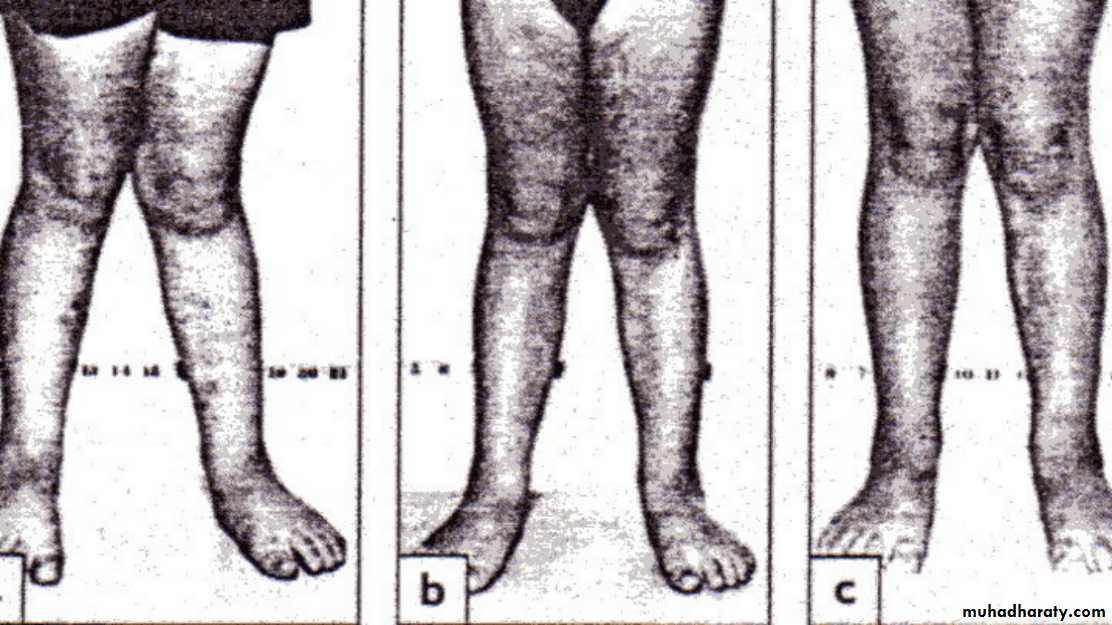
In normal adult the knee are in 5-7 degree valgus ; any deviation from this may regarded as deformity .The three common deformities are :
1- bow leg deformity (genu varum) .2- knock knee (genu valgum) .
3- hyper extension(genu recurvatum) .Causes of knee deformities:
1- physiological.2- ricketic.
3- idiopathic.
4-osteoarthritis.
5- rheumatoid arthritis.
6-mal united fractures around the knee.
7-infections (osteomyelitis or septic arthritis).8- Blount`s disease.
9- endocrinal e. g hypopituitarism.
10- Paget's disease.
Bow legs & knock knee
in babies are so common that are consider to be normal stage of development (physiological) ; in addition to this , rickets may play a role in developing these deformities physiological or renal rickets .
Bilateral bow leg
Measurement :
: distance between the femoral condyles with the legs held in full extension , and the heel touching ; it should beless than 6 cm .
Knock knee
The distance between the medial malleoli when the knee are held touching; it is usually
less than 8 cm .When the cause of the deformity is physiological .
it will be corrected spontaneously .And when caused by rickets it will be corrected by treating the rickets .
Surgical correction is indicated after this age by stapling or osteotomy usually after the age of 10 .
BLOUNT’S DISEASE
It is progressive bow leg deformity due to abnormal growth of the posteromedial part of the proximal tibia epiphysis , which is some time fragmented ;the metaphysis is some what beak shape .
The deformity is usually bilateral and it is progressive .
The treatment is by corrective osteotomy .
PATELLO-FEMORAL PAINSYNDROME (CHONDROMALACIAOF THE PATELLA
pain and tenderness in the anterior part of the knee.This syndrome is common among active adolescents and young adults.
It is often (but not invariably) associated with softening and fibrillation of the articular surface of the patella (chondromalacia patellae) .Treatment : conservative : by physiotherapy, analgesic anti inflammatory drugs.
Acute knee swellingCauses :
1 – haemoarthrosis .
2 – traumatic synovitis .
3 – acute septic arthritis .
4 – aseptic non traumatic synovitis .
Haemoarthrosis
Swelling immediately after the injury mean blood inside the joint .The knee is very painful and it feel warm, tense and tender …. Later there may be doughy feel .
X-ray : important to detect any fracture .
Treatment: aspiration under aseptic condition , crepe bandage and back slab , quadriceps ex. Start from the beginning .Traumatic synovitis
Injury stimulate reactive synovitis ,typically the swelling appear only after some hours and subside spontaneously over a period of days .
The knee may need to be splinted for several days , quadriceps ex.
Some time if fluid amount is large , it need aspiration .
Aseptic non traumatic synovitisAcute swelling without history of trauma or sign of infection , suggest gout or pseudo gout .
Aspiration from the joint show turbid fluid resembling pus but it is sterile
Microscopic ex. By polarized microscope show crystals .Treatment : by anti inflammatory drugs
Chronic swelling of knee
Causes :1 – T.B.
2 – Rheumatoid arthritis .
3 – Osteoarthritis .
Bursitis around the knee
1- Prepatellar bursitis( house maid’s knee).
It is uninfected bursitis .
not due to pressure , but to constant friction between skin and patella ;it is seen in carpet layers and miners .
Swelling is well circumscribed and fluctuant , joint is normal .Treatment
avoid kneeling
bandaging , occasionally aspiration;and in chronic case excision .
2- INFRAPATELLAR BURSITIS(clergyman’s knee) .The swelling is superficial to infrapatellar tendon (more distal to prepatellar bursitis) .
Gout may play a role in developing this type of bursa .
Treatment :the same as the prepatellar bursitisSemi membranous bursa
Normally there is bursa between the semimembranosus muscle and the medial head of the gastrocnemius muscle
This bursa may become enlarged and
the patient presented withpainless lump behind the knee slightly to the medial side of the midline
The joint is normal
Treatment :The bursa may disappear spontaneously , if not and there is pain then
excision should be done .
Differential diagnosis
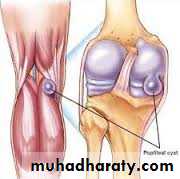
1- popliteal cyst .
Popliteal cystThis type of cyst is follow synovial rupture or herniation so the joint is abnormal ;
it may be osteoarthritis then the term BAKER’S CYST is applied or more commonly
rheumatoid in origin .
Usually the cyst is in the midline of the popliteal fossa .
Treatment :it is the treatment of the underlying causes ;
aspiration and injection of methylprednisolone is helpful .Excision is not advisable because recurrence is high , unless the underlying cause is treated
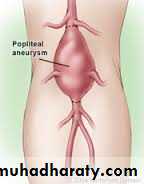
2. Popliteal aneurysm
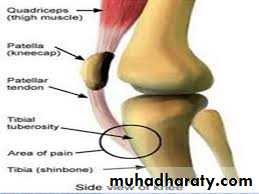
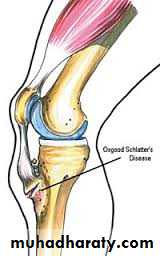
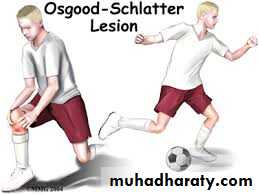
Osgood-schlatter’s disease
Apophysitis’of the tibia tubercleIt is a common disorder in which the
Tibia tubercle in adolescence become painful and swollen .It is also called osteochondritis of the upper tibia apophysis or apophysitis .
It is traction injury of the apophysis into which part of the patellar tendon is inserted .
It could be unilateral or bilateral
clinically
Young adolescent complains ofpain after activity
and of a lump.
The lump is tender and it’s situation over
the tibia apophysis is diagnostic .
X-ray
: show fragmentation of the apophysis.
Spontaneous recovery is usual but it take a time ; restriction of certain activities like cycling and soccer is advisable ;if no response then immobilization by p.o.p; if it
is more sever then surgery is indicated
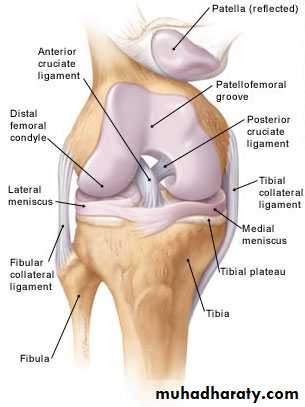
Knee injuries
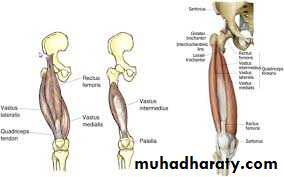
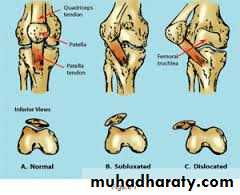
Knee joint (anatomical view)Dislocation of the patella
Because the knee is normally angled in slight valgus, there is a natural tendency for the patella to pull towards the lateral side when the quadriceps muscle contractd laterally by violence.Mechanism of injury :
sudden, severe contraction of the quadriceps muscle while the knee is stretched in valgus and external rotation.
Patients with joint hypermobility, valgus knee, muscle and joint abnormalities prone to this injury.
Clinically :
The knee collapses and patient fall on ground.
Patella can be felt on outer side of knee or the patella springs back into position spontaneously.
The X- ray
shows dislocation of patella laterally and associated fractures if present.
Treatment :In most cases the patella can be pushed back into place without much difficulty and anaesthesia is not always necessary.
A plaster slab is applied with the knee in extension for 3 weeks and quadriceps exercises.
However, if there is much bruising, swelling and tenderness medially, the patellofemoral ligaments and retinacular tissues are probably torn and immediate operative repair will reduce the likelihood of later recurrent dislocation.
Complication
Recurrences.
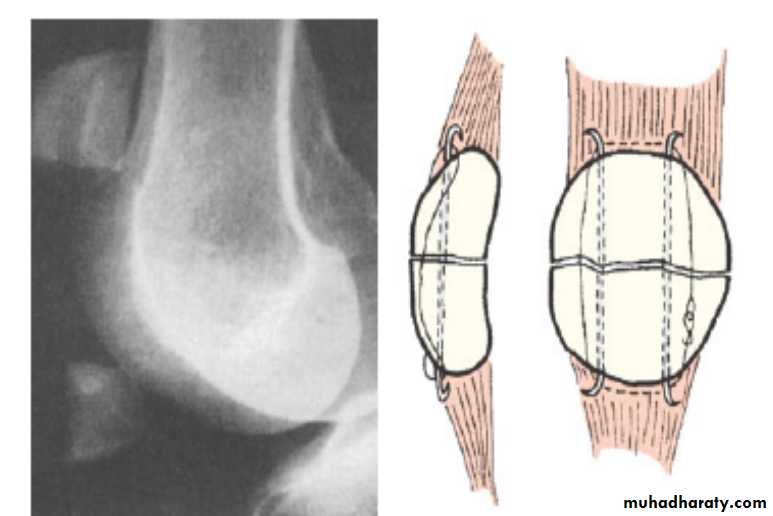
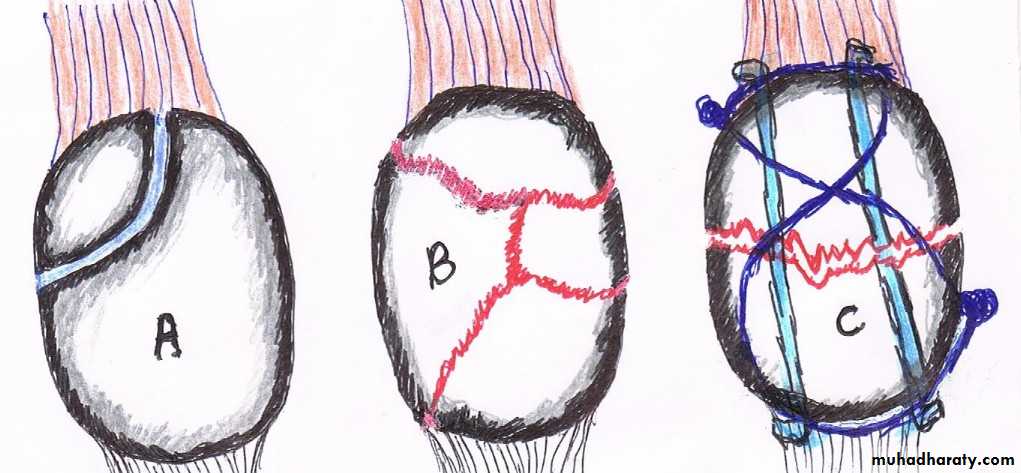
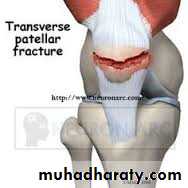
Fractures of patellait can be caused either by:
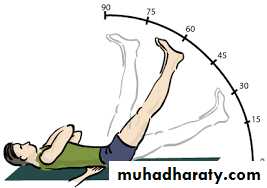
A- direct force :lead to undisplaced crack or comminuted fracture and here the extensor expansion usually remain intact (the patient can elevate straight leg).B- indirect force :
lead to transverse fracture with gap between the fragments Caused by resisted extension( sudden contraction of the quadriceps muscle against resistant ).
Associated with tears of collateral extensor expansions and failure of extensor mechanism (patient cannot elevate leg straight).
Treatment :
For the fractures caused by direct force :
In undisplaced or minimally displaced fracturesThe treatment is by p.o.p cylinder holding the knee straight should be applied for 3–4 weeks.
during this time quadriceps exercises are to be practised, haemoarthrosis should be aspirated. Severely comminuted and
displaced fracture
treated by
internal fixation or delayed patellectomy.
Internal fixation
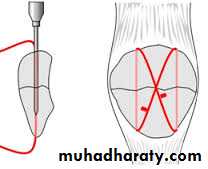
Indirect force:
Operation is essential.
Through a longitudinal incision the fracture is exposed and the patella repaired by the tension-band principle .The tears in the extensor expansions are then repaired.
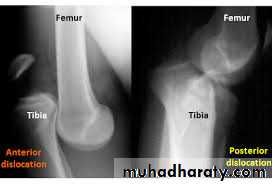
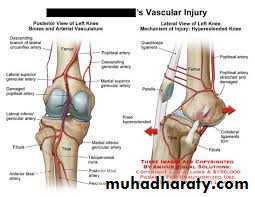
Knee dislocation
The knee can be dislocated only by considerable violence, as in a road accident.The cruciate ligaments
and one or both lateral ligaments are torn.There is sever swelling ,
bruisesand knee deformity.
The circulation and sensation in foot must be examined
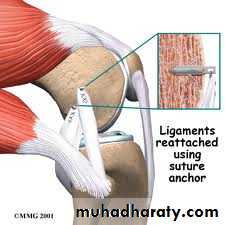
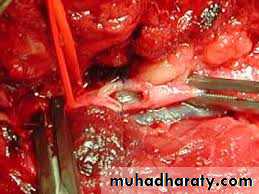
to exclude popliteal vessels and nerve injuriesTreatment :
URGENT reduction by closed or open reduction
followed bysplinting the knee in 15 degrees flexion for 12 weeks and
physiotherapy.Repeated check of circulation is essential,
If the joint is unstable anterior external fixator applied.If there is open wound or vascular injury the opportunity is taken to repair the ligaments and capsule.
When swelling subsides, a cast is applied for 12 weeks.
Quadriceps exercises encouraged from the start, and knee range of motion exercises after plaster removal.
Complications:
Early complications arearterial injures and nerve injuries.
Late complicationare chronic instability.
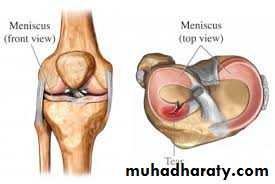
Meniscus injury
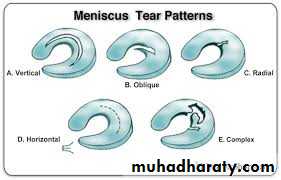
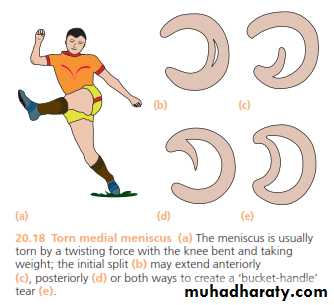
Meniscus injury are common in young adult especially football players, result froma twisting of semi-flexed or flexed knee.
The medial meniscus torn more than lateral meniscus.
The tear might affect the anterior or posterior horn of meniscus
as pedunculated tag ,or as bucket handle, sometimes
horizontal tears
or degeneration might occur.
Patients give
history of trauma,pain,
inability to extend knee
and delayed swelling of knee.
Locking
(in ability to fully extend the knee).
and unlocking are common feature of meniscus injury .
Diagnosis of meniscus
injury depend on
classical history
and clinical finding
ByMcmurray test.
MRI
is reliable method of diagnosis,
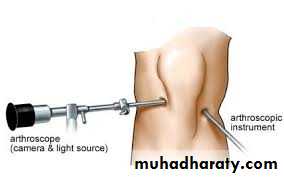
Arthroscopycan be used to confirm the diagnosis.
.Treatment
of choice is to remove the teared segment of meniscus arthroscopically.
Arthroscopic repair used for peripheral lesionsInjuries of the tibia
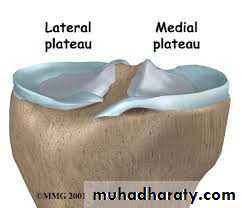
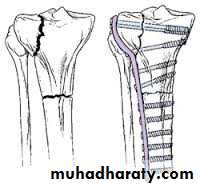
Tibial plateau fractures:Direct blow or fall from height may cause fracture of one tibial condyle or both.
Fracture lateral condyle is the commonest named as bumper fracture
caused by a force that abducts the tibia upon femur while the foot is fixed on ground.Patient usually is an adult, the knee joint is swollen, bruises, there is diffuse tenderness and doughy feel of haemarthrosis.
ligaments injuries must be excluded.
Imaging : X-ray
: anteroposterior, lateral & oblique views.
CT -Scan may used to detect amount of depression and comminuation.Tibial plateau fracture
Treatment:
Undisplaced fractures
treated conservatively:Haemarthrosis aspiration and compression bandaging,
above knee cast for one monthsfollowed by functional brace and physiotherapy.
For displaced fracturestreatment is by open reduction and internal fixation with
plate and screws as it is an intra articular fracture.fixation of tibial plateau fracture
Complications :
1- Vascular injuries and nerve injuries.
2- Compartment syndrome (specially with severe condylar fractures).
3- Joint stiffness (prevented by early range of motion exercises).4- Deformity
(Varus or Valgus), Valgus deformity are common complication.5- Secondary osteoarthritis (due to residual depression, knee deformity or ligament instability) .