1
Fifth stage
Medicine
Lec-8
د.فاخر
17/4/2016
Systemic lupus erythematosus
SLE is the most common multisystem connective tissue disease. It is characterized by a wide
variety of clinical features and a diverse spectrum of autoantibody production. The prevalence
varies according to geographical and racial background, from 30/100 000 in Caucasians to
200/100 000 in Afro-Caribbeans.
Aetiology and pathogenesis
wide spectrum of autoantibody production results from polyclonal B- and T-cell activation.
Many autoantigens in SLE are components of the intracellular and intranuclear machinery. In
normal health these antigens are 'hidden' from the immune system and do not provoke an
immune response
Etiological Factors & Pathogenesis
1- Genetic factors :
2
Family studies :
- High risk in siblings of SLE patients
- Up to 50% concordance in monozygotic twins .
- Healthy family members of SLE are more likely to have SLE type autoantibodies ( e.g. ANA
- Positive association of SLE with certain HLA-DR & DQ genes ( including HLA-DR2 & DR3 ) .
2-Environmental factors:
environmental factors that associate with flares of lupus-such as sunlight and artificial
ultraviolet (UV) light, pregnancy and infection-increase oxidative stress and subsequent
apoptosis
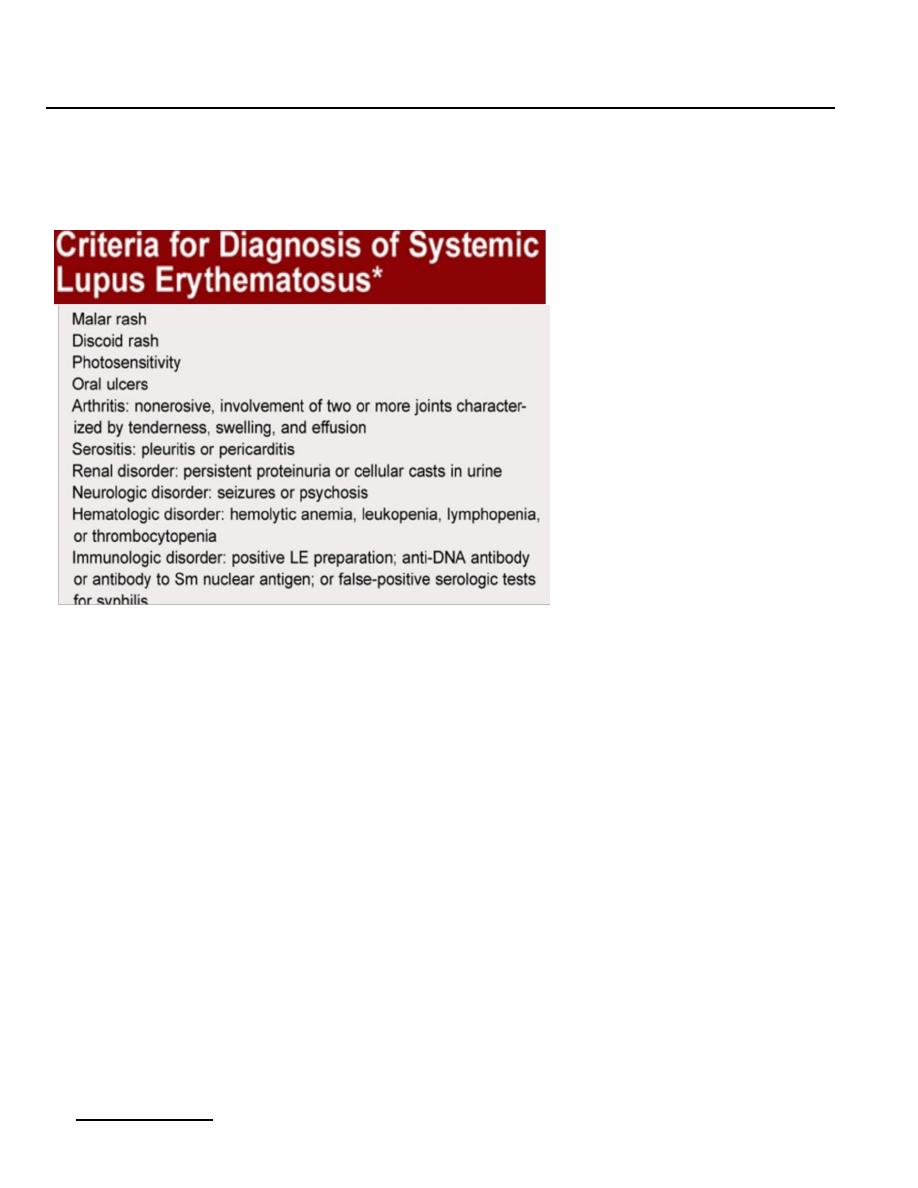
Clinical features
Arthralgia or arthritis in combination with Raynaud's phenomenon is the most common
presentation. It is important to elicit a history of Raynaud's since it is very uncommon for this
to associate with other arthropathies such as RA.
Raynaud's phenomenon in a teenage girl, with no other associated symptoms and especially if
there is a family history, is likely to be idiopathic 'primary' Raynaud's
A variety of joint problems may occur, including migratory arthralgia with mild morning
stiffness, tenosynovitis and small joint synovitis that may mimic RA. In contrast to RA, joint
deformities are rare. Deformities that do occur result from tendon inflammation and damage
rather than from bone erosion ('Jaccoud's arthropathy'
Mucocutaneous features
The classic butterfly facial rash (20-30% of patients) is raised and painful or pruritic and occurs
in a photosensitive distribution that spares the nasolabial folds.
Subacute cutaneous lupus erythematosus (SCLE) rashes are migratory, non-scarring and either
papulosquamous (psoriaform) or annular.
3
Discoid lupus lesions are characterised by hyperkeratosis and follicular plugging and may cause
scarring alopecia if present on the scalp.
Renal features
Renal involvement is one of the main determinants of prognosis, and regular monitoring of
urinalysis and blood pressure is essential. The typical renal lesion is a proliferative
glomerulonephritis, characterised by heavy haematuria, proteinuria and casts on urine
microscopy
Cardiopulmonary features
The most common manifestation is chest pain from pleurisy or pericarditis. Myocarditis and
sterile Libman-Sacks endocarditis may also occur,. SLE patients with antiphospholipid
antibodies are at
increased risk of venous thromboembolism, which should always be considered in the
presence of chest pain or dyspnoea. Alveolitis and lung fibrosis occur, particularly in overlap
connective tissue diseases
Central nervous system features
Fatigue, headache, poor concentration and other non-specific features similar to fibromyalgia
are common accompaniments of SLE and often occur in the absence of active disease. Specific
features of cerebral lupus include visual hallucinations, chorea (also associated with
antiphospholipid antibody syndrome), organic psychosis, transverse myelitis and lymphocytic
meningitis.
Haematological features
Antibody-mediated destruction of peripheral blood cells may cause neutropenia,
lymphopenia, thrombocytopenia or haemolytic anaemia. The degree of leucopenia, most
commonly lymphopenia, is often a good guide to disease activity. Although the ESR is usually
elevated, CRP is often normal unless there is serositis or infection.

4
Other manifestations
Fever, weight loss and mild lymphadenopathy commonly accompany active disease.
Gastrointestinal involvement is rare and other causes of abdominal pain should always be
considered, e.g. appendicitis, perforation secondary to drugs, or infection
Investigations:
The aims:
To confirm or exclude the disease .
To decide the extent of organ involvement .
To follow progression or regression of disease .
Treatment related investigations .
Commonly needed Investigations:
Organs evaluations : CBC , Renal functions with urine analysis , Liver functions , ECG
…etc .
Autoantibodies : next slide .
S. complement : oftenly reduced in active nephritis .
Partial thromboplastine time & prothrombine time .
Inflammatory markers : very high levels suggests infection .
Some autoantibodies in SLE:
ANA : positive in >95% . Poor specificity .
ds DNA antibody : positive in 30 – 50 % . High titer in SLE is specific . Oftenly correlates
with activity .
Anti- Sm antibody : positive in 25% . High specificity .
Anti- Ro antibody in 25% , may be positive in ANA -ve cases & in neonatal lupus .
Antiphospholipid antibodies .

5
Management
Medication
* Topical agents :
- Sun protection factor (25 – 50) with sun avoidance .
- Topical steroids .
* NSAID : limitations in renal & GIT problems .
* Chloroquine : for skin & joint lesions & ? Others .
* Aspirin : ( low dose) for thrombotic vascular disorders & fetal losses .
* Heparin / Warfarin .
* Corticosteroids :
- Pulse therapy .
• Acute or life-threatening disease (i.e. renal, cerebral) requires high-dose corticosteroids
(e.g. oral prednisolone 40-60 mg daily or i.v. methylprednisolone 500 mg-1 g) in
combination with pulse i.v. (10 mg/kg IV), coupled with cyclophosphamide
• (15 mg/kg IV), repeated at 2–3-weekly
- Oral therapy . Dose according to condition .
* Immunosupressive / cytotoxic therapy :
- Cyclophosphamide .
- Azathioprine .
- Mycophenolate mofetil .
- MTX , ciclosprine A …
* Osteoporosis prevention & hypertension treatment .

6
Prognosis
With effective therapy the 5 years survival exceeds 90% & 10 years survival exceeds 70%
Delayed treatment of nephritis is associated with high mortality .
Lupus nephritis occurs in 10% of transplanted kidneys in SLE cases .
Drugs Induced Lupus
Blamed drugs include beta-blockers , angiotensine converting enzyme inhibitors , INH ,
minocycline , TNF blockers , sulfasalazine …etc .
ANA usually positive .
Renal , CNS involvements & dsDNA antibody are all rare .
Usually resolve within weeks after stopping the drug .
