1
Fifth stage
Dermatology
Lec-18
.د
عمر
18/4/2016
Benign Skin Lesions
Overview of Benign Skin Lesions:
Most skin lesions are benign; however, some concern has caused the patient to make
an inquiry, and a correct diagnosis is important.
The following 3 general types of characteristics must been considered when defining a
benign lesion:
1. Characteristics outside of the lesion e.g. patient age, ethnicity, presence of
associated symptoms, related systemic disorders, and location.
2. Physical characteristics of the lesion
3. Histologic characteristics of the lesion
Initially, benign lesions must be differentiated from malignant lesions. This is best done
by being familiar with characteristics of common malignant lesions.
The clinician should try to categorize any skin lesion as one of the following:
4. most likely benign,
5. most likely malignant,
6. or unclear.
the last 2 categories should be biopsied.
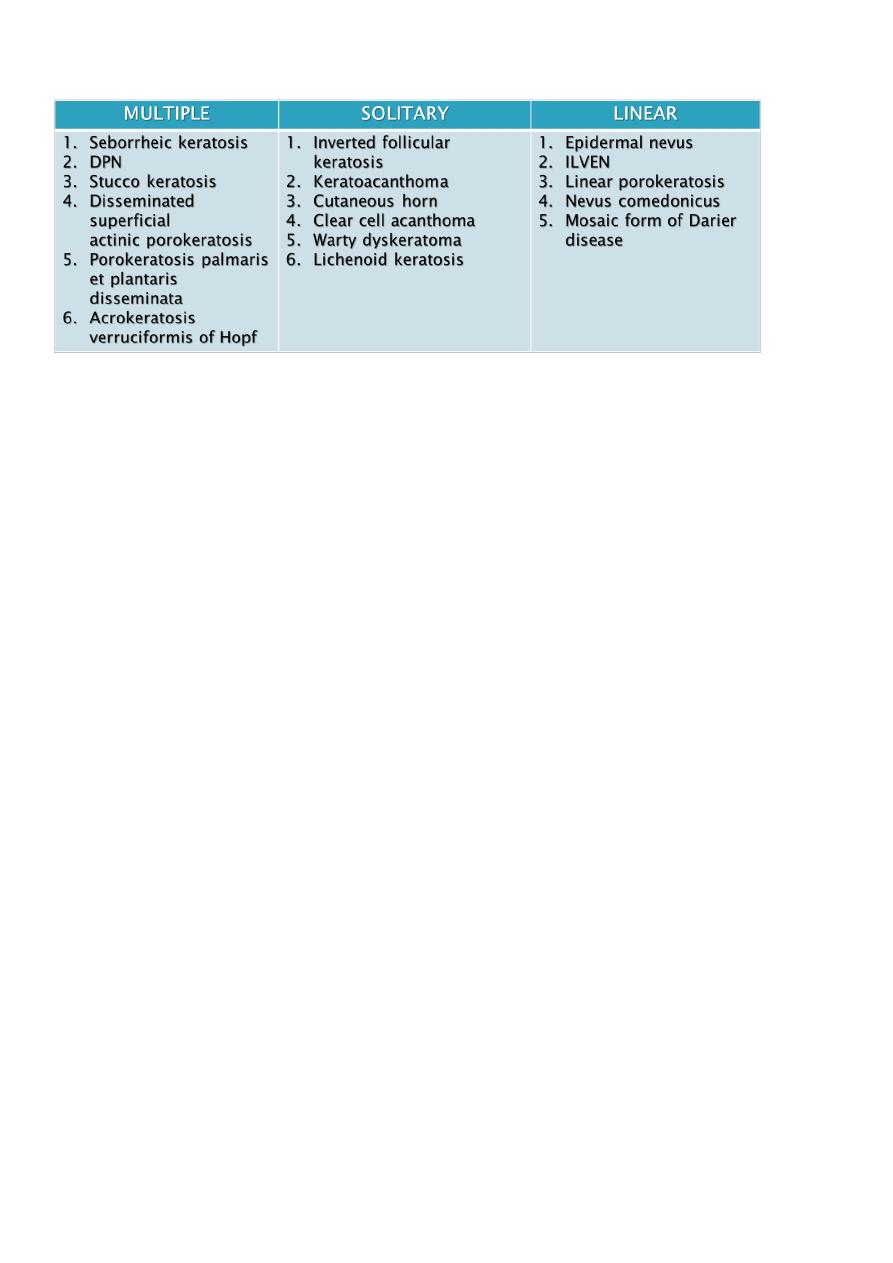
Classification of Benign lesions of the skin:
Benign lesions of the surface epithelium.
Cutaneous Cysts.
Benign Melanocytic Neoplasms
Neoplasms and proliferations of follicular lineage
Neoplasms and proliferations with sebaceous differentiation
Neoplasms and proliferations with apocrine differentiation
Neoplasms and proliferations with eccrine differentiation
Fibrous and Fibrohistiocytic Proliferations of the Skin and Tendons
Muscle, Adipose and Cartilage Neoplasms
Vascular Neoplasms
2
Benign Epidermal Proliferations:
Seborrheic keratosis:
SKs usually begin to appear during and after the fourth decade and continue to arise
throughout life.
An apparent familial predisposition with a postulated autosomal dominant inheritance.
They only occur on hair bearing skin. Can arise on all body surfaces except mucosa,
palms and soles.
Though harmless, SKs can occasionally become irritated or can be cosmetically
bothersome.
Pathogenesis of SKs:
The exact cause of seborrhoeic keratoses is not known may be;
1. There is a familial predisposition in those with hundreds of lesions.
2. Sun exposure (Although SKs are common in areas covered by clothing) higher
prevalence of SKs within sun-exposed areas such as the head and neck in contrast to
non-sun exposed areas in the same subjects.
3. Very rarely, eruptive SKs may denote an underlying internal malignancy. The syndrome
is known as the sign of Leser-Trélat.
4. Neoplastic origin (somatic mutations).
5. HPV may be implicated.
C/P of SKs:
Typically appear as sharply marginated, pigmented lesions.

3
They may be macules, papules, plaques or even pedunculated, depending on their
stage of development.
Color is variable even within the same lesion (pink, yellow, flesh colored, tan, brown,
black).
Surface is usually waxy and the texture can vary from smooth, velvety to verrucous.
Often multiple & can be extensive.
Keratotic plugging with follicular prominence.
They have a stuck-on quality.
SKs can develop on the face, neck and trunk (especially the upper back), as well as the
extremities.
Usually measure about 1 cm in diameter but they can become quite large, i.e. > 5 cm in
diameter.
Lesions may become inflamed due to rupture of the small pseudocysts they contain or
from trauma, or rarely from infection with microorganisms such as Staphylococcus
aureus.
Conditions associated with an abrupt “flare” of lesions followed by regression include
pregnancy, coexisting inflammatory dermatoses (in particular erythroderma) and
malignancy.
How can I tell if a lesion is a SKs?
If you are in doubt of the diagnosis, try gently picking or scratching the lesion. It may
crumble, hyperkeratotic scale, or lift off, revealing that superficial waxy character.
C/P of SKs:
Use dermoscopy to look for keratin pseudocysts.
These are small white spots commonly found in seborrheic keratoses.
SKs and Malignancy:
It is not precancerous.
SCC cutaneous melanoma, BCC, keratoacanthoma, and SCC in situ have all been rarely
observed in association with SKs. This represents a coincidental neoplasm developing
in adjacent skin.
The sign of Leser–Trélat is a rare cutaneous marker of internal malignancy (in particular
gastric (60%) or colonic adenocarcinoma, breast carcinoma, and lymphoma). It is
considered to be a paraneoplastic cutaneous syndrome characterized by an abrupt and
striking in the number and/or size of SKs occurring before, during or after an internal
malignancy has been detected majority and of the lesions are located on the back,

4
followed by the extremities, face and abdomen and usually associated with pruritus.
Neoplasm may secrete TGF-alpha epithelial hyperplasia.
Clinical Variants of SKs:
IRRITATED SEBORRHOEIC KERATOSIS
DERMATOSIS PAPULOSA NIGRA
STUCCO KERATOSES
INVERTED FOLLICULAR KERATOSES
I. Irritated SKs
Inflamed lesion, often red, edematous and crusted.
II. Dermatosis Papulosa Nigra (DPN)
Multiple, small, symmetric hyperpigmented, sessile to filiform, smooth-surfaced
papules measuring from 1 to 5 mm.
Arise in darker skin types, usually on the cheeks, temples. Less often, lesions are on
the neck, chest and back.
It has a strong familial predisposition. Women are twice as likely to be affected as men.
It tends to have an earlier age of onset (during adolescence) than that of SKs.
HP pattern quite similar to the acanthotic type of SK.
III. Stucco keratosis
Small white-gray papules or plaques scattered on dorsal feet and ankles of older fair-
skinned individuals.
Lesions are “stuck on”, and when scraped off, with a fingernail and there is usually
minimal, if any, bleeding. A collarette of dry scale may remain
The papules may number in the hundreds. They are usually small, measuring from 1 to
4 mm, but rarely individual plaques may be as large as a few centimeters.
There is no familial predilection.
Men are four times more likely to be affected than women.
It displays prominent orthokeratotic hyperkeratosis and papillomatosis, often showing
“church spire” pattern.
IV. Inverted Follicular Keratosis (IFK)
Asymptomatic solitary firm, white to light-tan or pinkish papules usually less than 1 cm
in diameter on face or neck of middle-aged and older adults.
They are typically stable and persistent lesions, but may regress.
Benign endophytic variant of irritated SK.
5
It is derived from the infundibulum of the hair follicle.
Histologically, The keratinocyte proliferation seems to surround one or several
follicular canals that open to the surface. squamous eddies and inflammation are
common.
HP of SKs:
There are at least six histologic types of SK but different histologic features are often
present in the same lesion:
1. Acanthotic: the most common.
2. Hyperkeratotic: more prominent hyperkeratosis and papillomatosis.
3. Reticulated: delicate strands of epithelium that extend from the epidermis in an
interlacing pattern.
4. Irritated: perivascular, diffuse or lichenoid lymphoid infiltrate. Squamous eddies
are common findings.
5. Clonal: well defined nests of loosely packed uniform cells in the epithelium.
6. Melanoacanthoma: shows dendritic melanocytes packed with melanin which is
absent in keratinocytes.
The acanthotic type:
Usually presents as a smooth surfaced, dome shaped papule. Slight hyperkeratosis and
papillomatosis are often present, while the greatly thickened epidermis typically
contains a preponderance of basaloid cells.
Sharply demarcated horizontal base called “string”.
Papillae may be narrow in some lesions.
Invaginated horn pseudocysts are most prevalent in this variant.
This type often contains an amount of pigment superior in quantity than others; it is
primarily concentrated in keratinocytes and is transferred from neighboring
melanocytes and deeply pigmented lesions contain abundant melanin in basaloid cells.
Hyperkeratotic type:
with church spires of papillomatosis and hyperkeratosis & preponderance of squamous
cells relative to basaloid cells

6
Reticulated type:
with delicate, lace-like strands of interconnecting epithelium composed of a double row or
more of hyperpigmented basaloid cells and interspersed horn pseudocysts
Irritated type:
exophytic lesion with papillomatosis, hyperkeratosis, hemorrhagic crust
and dermal inflammation
Clonal type:
with Borst–Jadassohn phenomenon* characterized by well-demarcated nests of
keratinocytes within the epidermis
* ‘clones’ of basaloid, squamatized, or pale keratinocytes in epidermis appear different
than their neighbors
Treatment of SKs:
Assurance.
Superficial destructive means mainly for cosmetic reasons;
1. Cryotherapy: The most commonly used method but can result in
hypopigmentation in dark individuals.
2. Curettage.
3. Electrodessication (very light) is often safe.
4. Shave excision
5. Scissor snip (pedunculated lesions & DPN).
6. Laser ablation (pulsed CO2, erbium: YAG)
Full thickness excision: if melanoma is considered in the differential diagnosis for
histology.
