1
Fifth stage
Dermatology
Lec-22
.د
عمر
18/4/2016
MALIGNANT MELANOMA
Outline:
Introduction
Aetiology
Types
Invasion and Metastasis
Risk Factors
Diagnosis and Staging
Treatment and Prevention
Skin:
Epidermis – Melanocytes
• Melanocytes:
– In stratum basale
– Pale “halo” of cytoplasm
– Neural crest
– Produce melanin and pass it on to nearby keratinocytes
– Melanin covers nuclei of nearby keratinocytes
– Skin colour depends on melanocytes activity, rather than the number present
MALIGNANT MELANOMA:
• A tumour arising from melanocytes of the basal layer of the epidermis
• Less commonly – uveal tract (eye) and meningeal membranes
AETIOLOGY
• The cause is unknown.
2
• Excessive exposure to sunlight
• Genetic predisposition
RISK FACTORS FOR MELANOMA:
• Large numbers of benign naevi
• Clinically atypical naevi
• Severe sunburn
• Early years in a tropical climate
• Family history of MM
Clinical features:
• Occur anywhere on the skin
– Females (commonest is lower leg)
– Males ( back).
• Early melanoma is pain free. The only symptom if present is mild irritation or itch.
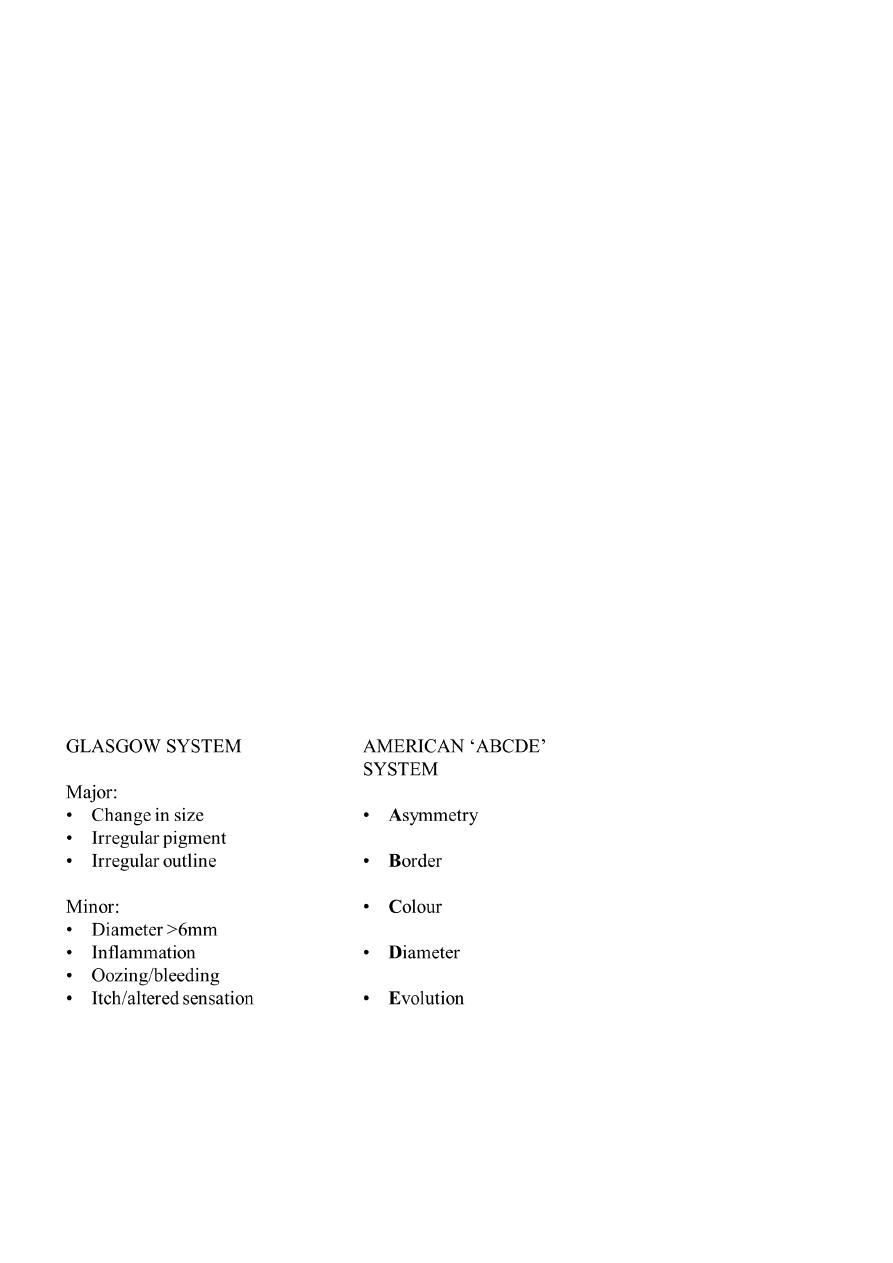
AIDS IN CLINICAL DIAGNOSIS:
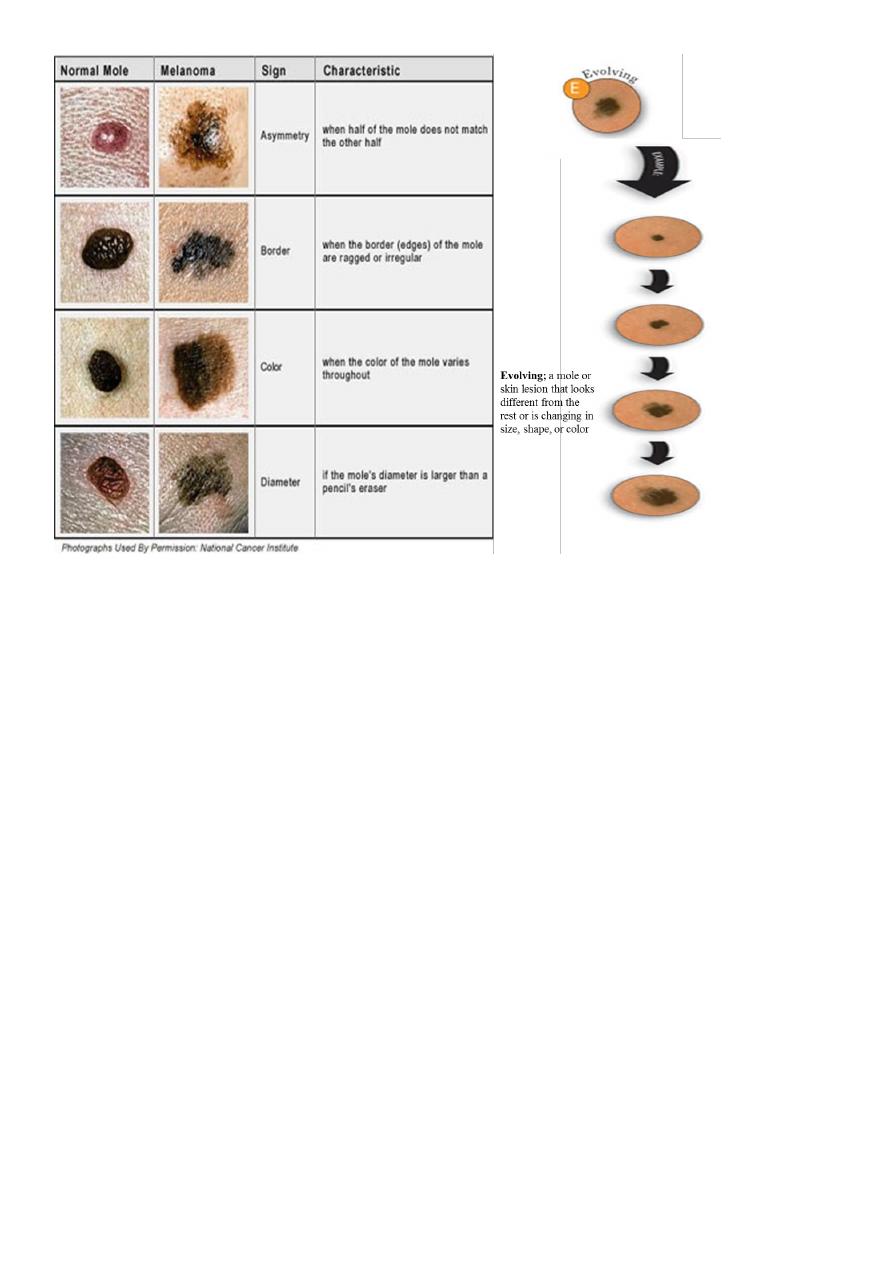
3
TYPES OF MELANOMA:
• Superficial spreading Malignant melanoma
• Nodular melanoma
• Letingo maligna melanoma
• Acral malanoma
SUPERFICIAL SPREADING:
• The most common type of MM in the white-skinned population – 70% of cases
• Commonest sites – lower leg in females and back in males
• In early stages may be small, then growth becomes irregular
NODULAR:
• Commoner in males
• Trunk is a common site
• Rapidly growing

4
• Usually thick with a poor prognosis
• Black/brown nodule
• Ulceration and bleeding are common
ACRAL LENTIGINOUS MELANOMA:
• In white-skinned population this accounts for 10% of MMs, but is the commonest
MM in nonwhite-skinned nations
• Found on palms and soles
• Usually comprises a flat lentiginous area with an invasive nodular component
SUBUNGAL MELANOMA:
• Rare
• Often diagnosed late – confusion with benign subungal naevus, paronychial
infections, trauma
• Hutchinson’s sign – spillage of pigment onto the surrounding nailfold
LENTIGO MALIGNA MELANOMA:
• Occurs as a late development in a lentigo maligna
• Mainly on the face in elderly patients
• May be many years before an invasive nodule develops
DDx:
• Superficial spreading melanomas
Benign melanocytic naevi.
• Nodular melanomas
Vascular tumor
Histiocytoma
• Latingo maligna melanoma
Seborrhic keratoses
5
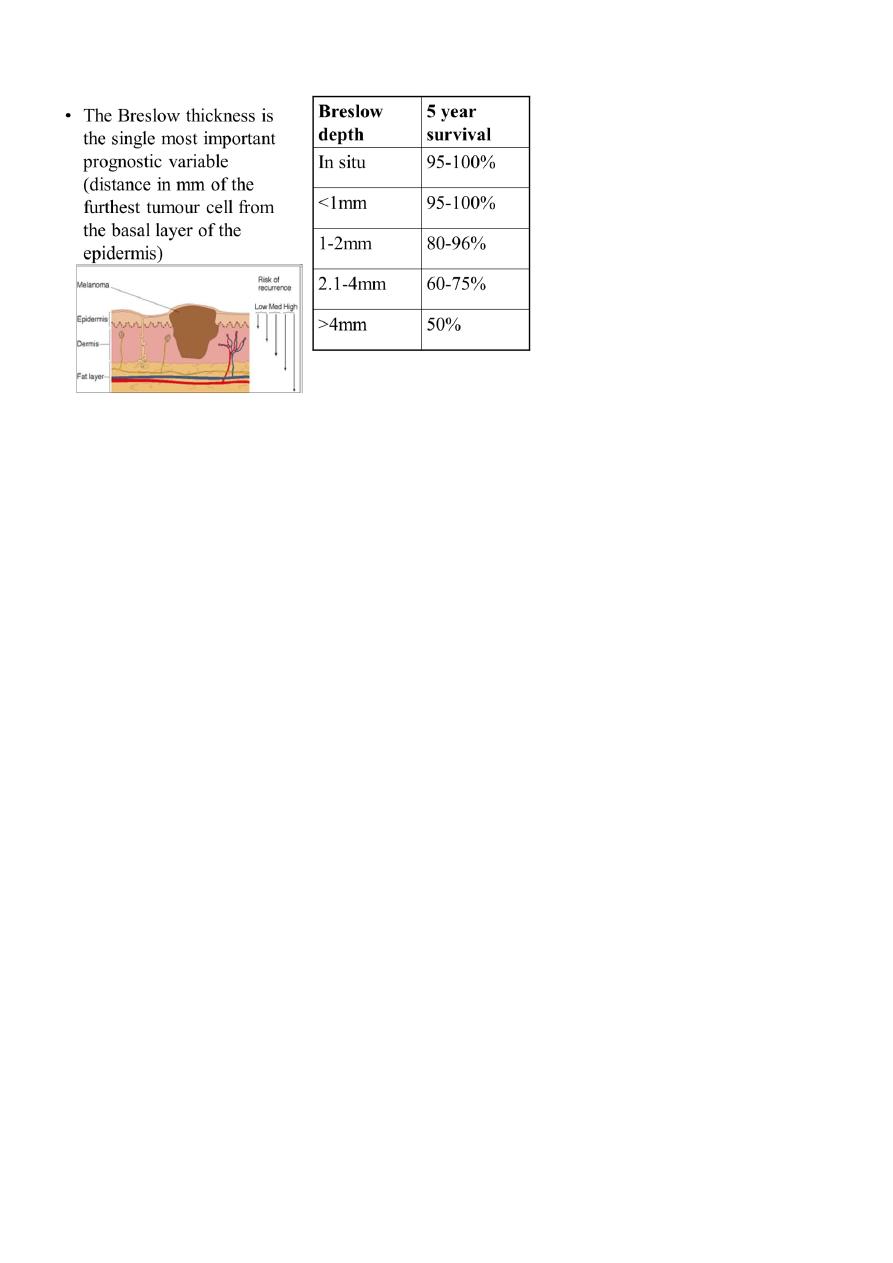
PROGNOSTIC VARIABLES:
• Scalp lesions worse prognosis, then palms and soles, then trunk, then extremeties
• Younger women appear to do better than either men at any stage or women over 50
• Ulceration of the tumour surface is a high risk factor
MANAGEMENT:
• Surgical resection of tumour
• MOHS technique
• Lymph node dissection
• Chemotherapy
• Radiotherapy
• Immunotherapy
Prevention:
• Reduce risk factor exposure:
• Covering up (sunscreen, sunglasses, clothes)
• Avoidance (less time in sun)
• Screening (possibly feasible)
