11/27/2012
1Good afternoon
11/27/20122
Keratoconus
It is ectatic progressive disorder in which the cornea assume a conical shape secondary to stromal thing & protrusion.The onset is around puberty with slow progression thereafter until the third or fourth decades of life, when it usually arrest.
11/27/2012
3
Presentation:
Is typically during puberty with unilateral impairment of vision due to progressive myopia & astigmatism, which subsequently become irregular.The patient may report frequent changes in spectacles prescription or decrease tolerance
to contact lens wear.Approximately 50% of normal fellow eyes will progress to Keratoconus within 10 years.
11/27/20124
11/27/2012
5Progressive corneal thinning
1- Signs:
Direct ophthalmoscopy from a distance of one foot shows anoil droplet reflex.
Retinoscopy shows an irregular scissor reflex.
Slit-lamp biomicroscopy shows fine, vertical deep stromal striae (Vogt lines) which disappear with external pressure on globe.
Epithelial iron deposits may surround the base of the cone ( Flescher ring) best seen with
cobalt blue filter.
Progressive corneal thinning to as little as one third of normal thickness associated with poor visual acuity resulting from marked irregular myopic astigmatism.
Bulging of lower lid in down gaze ( Munson sign).
11/27/20126
Signs of keratoconus
Bilateral in 85% but asymmetricalOil droplet reflex
Prominent corneal nervesVogt striae
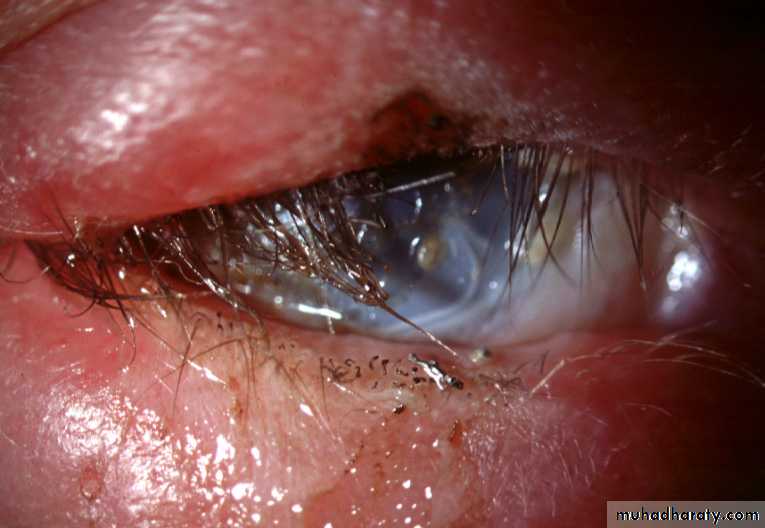
Acute hydrops
Munson signFleischer ring & scarring
Bulging of lower lids
on down gazeCorneal topography:
shows irregular astigmatism and is the most sensitive method of detecting early Keratoconus & monitoring progression.11/27/2012
8
Acute hydrops
Is caused by rupture in Descemet membrane that show influx of aqueous into the cornea . This cause sudden drop in visual acuity associated with discomfort & watering.Although breaks usually heals within 6-10 weeks & corneal edema clears a variable amount of stromal scarring may develop. Acute episodes are initially treated with hypertonic saline & patching of soft bandage contact lens.
Healing may result in improved visual acuity as a result of scarring & flattening of the cornea. Keratoplasty should be deferred until the edema resolved.
11/27/2012
9Manual Placido disc
11/27/201210
Computerized topography
11Irregular configuration
Association:
1- Systemic disorders: include Down, Turner , Ehler-Donalos ,Marfan syndromes ,atopy , osteogenesis imperfecta , mitral valve prolapse and mental retardation.2- Ocular associations: include vernal keratoconjunctivitis, blue sclera , aniridia, ectopia lentis ,Leber congenital Amaurosis and retinitis pigmentosa.
11/27/2012
12
Systemic associations of keratoconus
Crouzon syndrome
Marfan syndromeAtopic dermatitis
Down syndromeEhlers-Danlos
syndrome
Treatment;
1- Spectacles: in early cases to correct irregular astigmatism .2- Rigid contact lenses: are required for higher degree of astigmatism to provide a regular refracting surface.
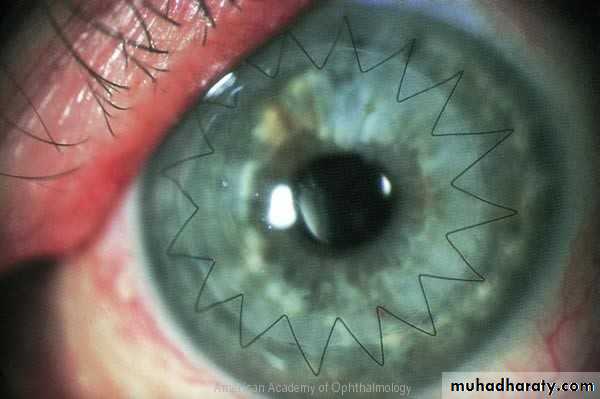
3- Keratoplasty, (penetrating or deep lamellar) is indicated for patients with advanced progressive disease especially with significant corneal scarring.
11/27/2012
14
Other surgical options:
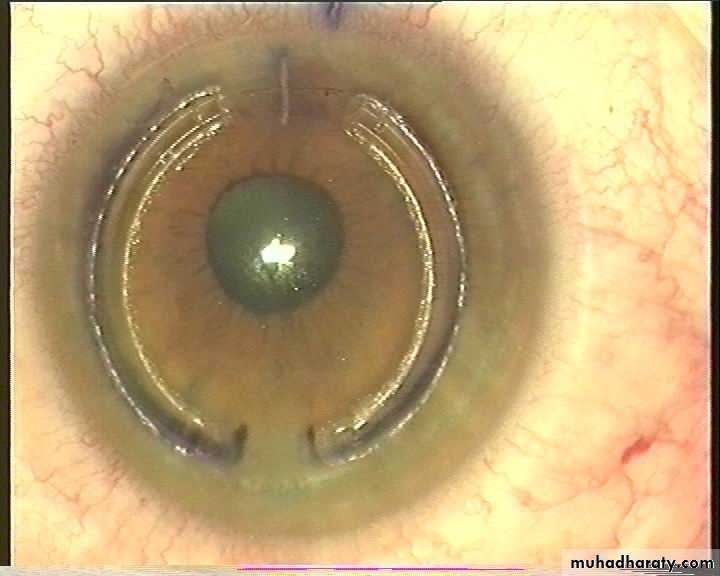
Intracorneal ring implantation (INTACS)
Corneal Collagen cross- linking.
11/27/2012
15
11/27/2012
16Technique of penetrating Keratoplasty
Corneal injuries
Corneal abrasionCorneal foreign body
Radiation damage
Chemical injuries
11/27/2012
18
Corneal abrasion
Are the most common ,Result of blunt injury, they may follow injuries with foreign bodies , finger nails and twigs.
Abrasions will be missed if Flurescein is not instilled.
11/27/201219
The aims of treatment
• To ensure healing of the defect.• Prevent infections.
• Relive pain.
11/27/2012
20
11/27/2012
21
Small abrasions can be treated with chloramphenicol ointment twice a day or eye drops q.i.d.
Large abrasions : double eye pads with chloramphenicol ointment, the pad must be firm enough to keep the eyelid shut.
11/27/2012
22
If there is significant pain; cycloplegic eye drop (e.g. cyclopentolate 1%) may help.
Oral analgesics , such as paracetamol and NSAIDs can also be used.Patient should seek further ophthalmological help if the eye continue to be painful, vision blur, or development of purulent discharges.
11/27/2012
23
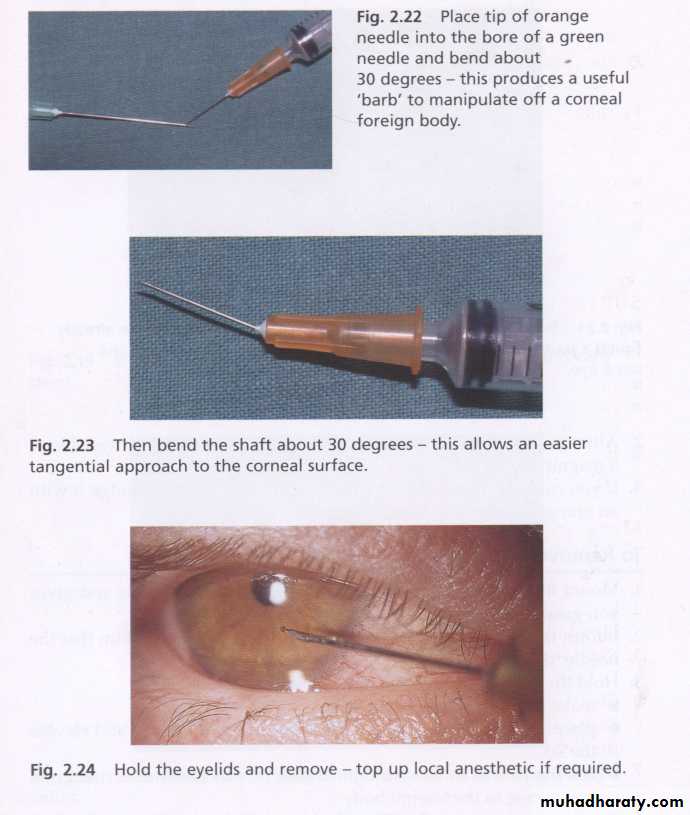
Corneal foreign body
A patient may not recall a foreign body having entered the eye, so it is essential to be on the lookout for a foreign body if the patient has an uncomfortable red eye.Local anesthetics to examine eye and remove foreign body .
11/27/2012
24
Corneal foreign body
Local anesthetics should never be given to patients themselves, because they impede healing & further injuries may occur to anaesthetized eye !!!
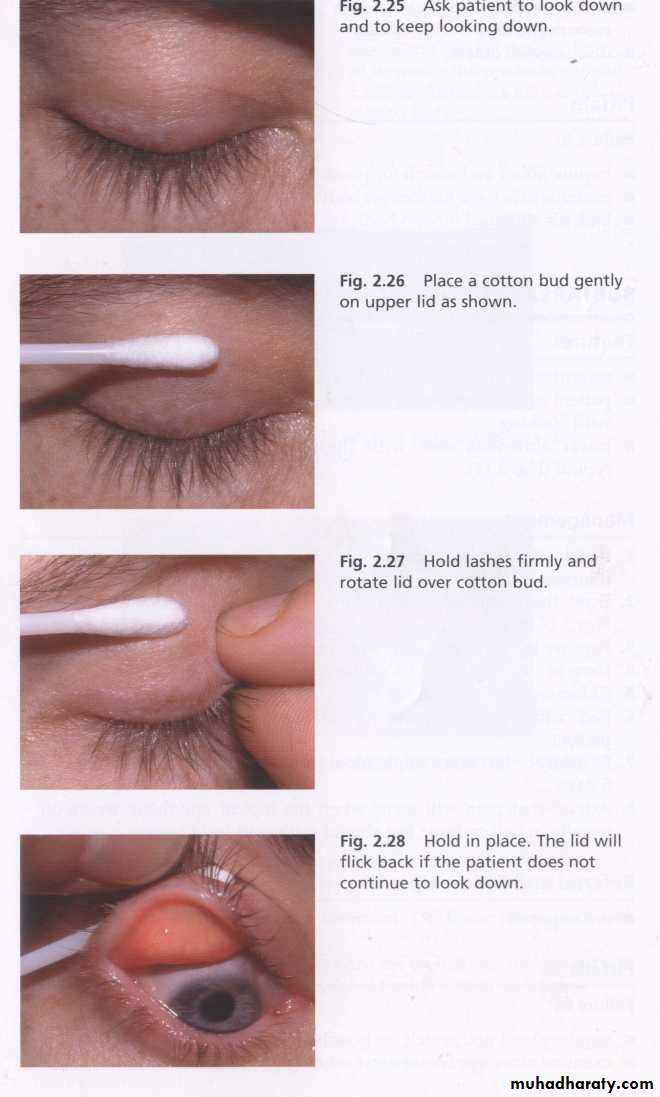
The upper lid must be everted to exclude a sub-tarsal F.B, particularly if there is corneal scratches or a continuing feeling that a F.B is present.
11/27/2012
26
Corneal F.B are often more difficult to remove if they are metallic because they are often “Rust on”.
They must be removed as they will prevent healing & may permanently stain the cornea.
11/27/201227
A cotton wool bud can be used for removal of F.B , but great care must be taken when using this as the eye may easily be damaged.
If there is any doubt ,those patients should be referred to an Ophthalmologist.
When the F.B has been removed ,any remaining epithelial defect remains can be treated as abrasion.
11/27/2012
28
Please evert the upper lid
Scan the cornea carefullyRadiation damage
The most common form of radiation damage occur when welding has been carried out without adequate shielding of the eye.The corneal epithelium is damaged by ultraviolet rays & patient typically presents with painful weeping eyes some hours after welding & commonly known as “ Arc eye”.
Treatment : as for corneal abrasion.
11/27/2012
32
Chemical injuries
All chemical eye injuries are potentially blinding injuries.If chemicals are splashed into the eye, the eye & the conjunctival sacs(fornices) should be washed out immediately with copious amount of water.
11/27/2012
33
Acute management should consist of three “Is Irrigate , Irrigate , Irrigate “.
Alkali are potentially damaging & any loose bits such as lime should be removed from the conjunctival sac with the aid of local anesthetics if necessary.11/27/2012
34
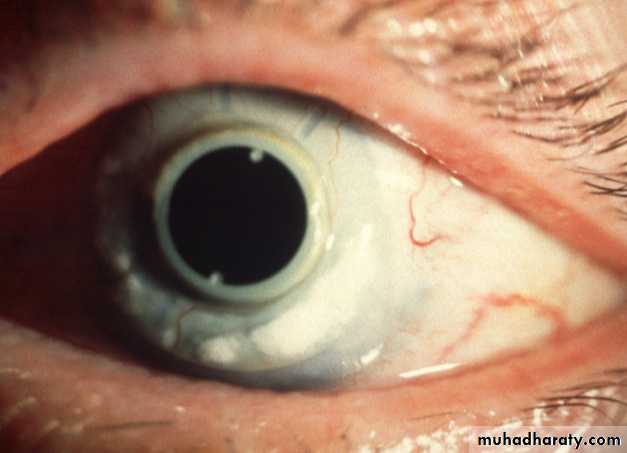
Chemical injury/ limbal ischemia
11/27/2012
35Management
• Copious irrigation to neutralize PH.• Double evertion of eyelid , so that any retained particulate matter may be removed.
• Debridement of necrotic area of corneal epithelium to allow for proper re-epithelialization.
11/27/2012
36
Medical treatment
• Short coarse of steroid 7-10 days.• Cycloplegics (cyclopentolate 1%).
• Prophylactic antibiotics for about 7-10 days.
• Ascorbic acid : it improves wound healing topical Sod. Ascorbate 10% is given 2 hourly in addition to systemic dose of 2 grams q.i.d.
• Citric acid : reduce intensity of inflammatory response (topical Sod.citrate 10% 2 hourly for 10 days).
• Tetracycline :effective collagenase inhibitors & inhibits neutrophils activities and reduce ulceration.
• Doxcycycline 100 mg b.d.
11/27/2012
37
Grading of severity of chemical injuries
Clear cornea
Grade I (excellent prognosis)
Limbal ischemia - nil
Cornea hazy but visible iris details
Grade II(good prognosis)
Limbal ischemia < 1/3
No iris details
Grade III (guarded
prognosis)
Limbal ischemia - 1/3 to 1/2
Opaque cornea
Grade IV (very poor
prognosis)
Limbal ischemia > 1/2
Surgical treatment of chemical injuries
Division of conjunctival bandsCorrection of eyelid deformities
Treatment of corneal opacity by
keratoplasty or keratoprosthesis
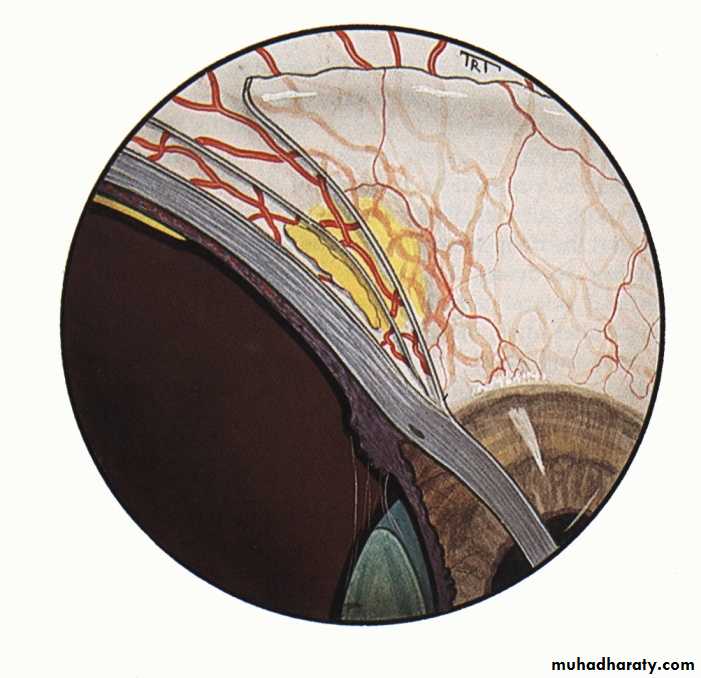
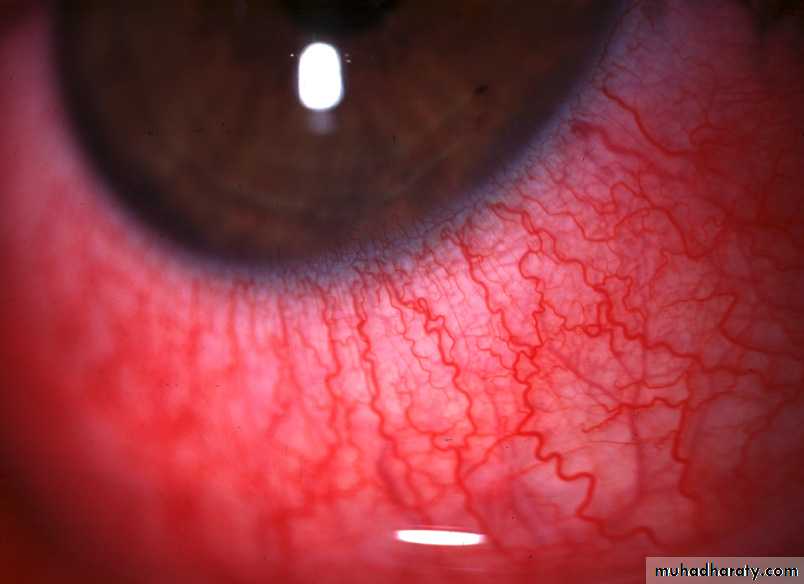
Applied anatomy of vascular coats of outer tunic
ScleritisMaximal congestion of deep vascular plexus
Slight congestion of
episcleral vessels
Maximal congestion
of episcleral vessels
Episcleritis
Normal
Radial superficial episcleral vessels
Deep vascular plexus
adjacent to sclera
11/27/2012
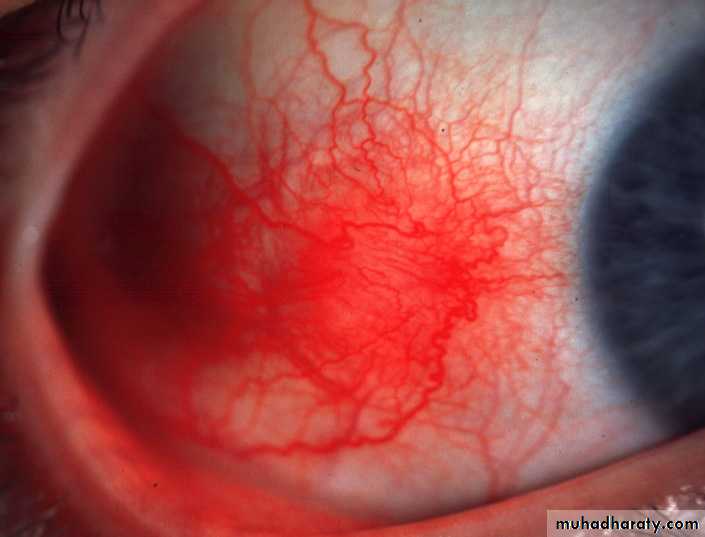
41Simple episcleritis
Common, benign, self-limiting but frequently recurrentTypically affects young adults
Treatment
Seldom associated with a systemic disorder
Simple sectorial episcleritis
Simple diffuse episcleritis
Topical steroids
Systemic flurbiprofen ( 100 mg tid if unresponsive)
Scleritis
Scleritis is characterized by edema and cellular infiltration of the entire thickness of the sclera.It is less common than episcleritis.
It Covers a spectrum ranging in severity from self-limiting episodes to necrotizing disease threatening the vision.
Diffuse anterior non-necrotizing Scleritis
Widespread scleral and episcleral injectionRelatively benign - does not progress to necrosis
Oral steroids if unresponsive
Treatment
Oral NSAIDs
Causes and Systemic Associations of Scleritis
1. Rheumatoid arthritisWegener granulomatosis
Polyarteritis nodosa
Systemic lupus erythematosus
2. Connective tissue disorders
3. Miscellaneous
Relapsing polychondritis
Herpes zoster Ophthalmicus
Surgically induced
Treatment of Scleritis
1- Topical steroids
2- Systemic NSAIDs
3- Periocular steroid injections
4- Systemic steroids
5- Cytotoxic agents
Cyclophosphamide,azathioprine,methotrexate.
6-Immune modulators: Cyclosporine & tacrolimus.
MCQ sample:
The definitive treatment for keratoconus:A- corneal collagen cross-linking
B- intracorneal ringsC- corneal graft
D- soft contact lenses
11/27/2012
47
11/27/2012
48Thank you for your attention