1
Fifth stage
ENT
Lec-20
د.سعد
21/4/2016
VERTIGO
There are 4 types of Dizziness:
1. Vertigo
2. Lightheadedness.
3. Presyncope.
4. Disequilibrium.
Disorders of vestibular system cause vertigo.
Vertigo accounts for 54% of all dizziness; Vertere = Spin (Latin).
Vertigo is an illusion of movement of the patient’s body or patient’s environment. It should
be restricted to sensation of rotation and linear motion (staggering to one side). Severe
vertigo is more commonly caused by peripheral vestibular lesions.
Aetiology:
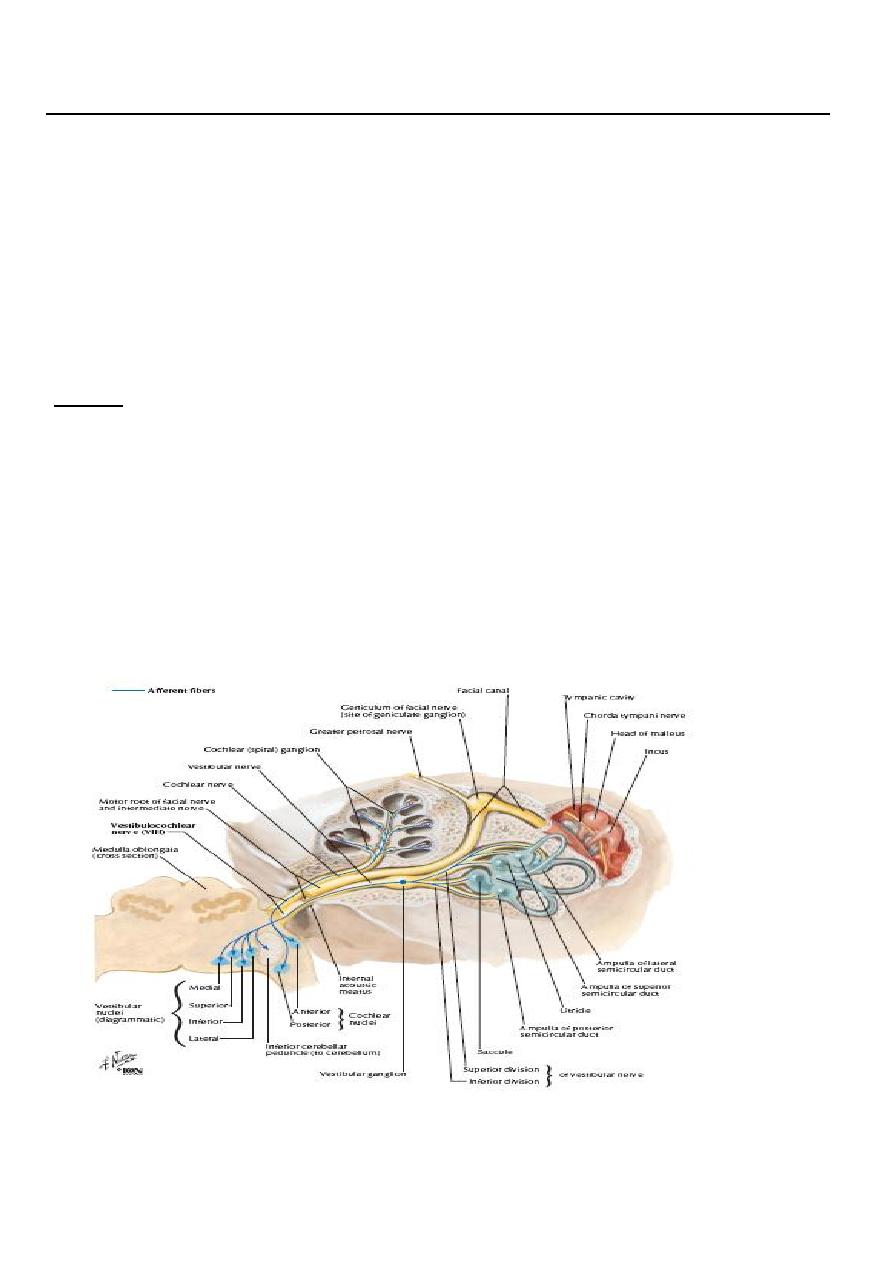
A. Central ( non-otological) which involve the CNS after the entrance of the vestibular
nerve in the brainstem e.g. intracranial tumors, multiple sclerosis, vestibulobasillar
ischaemia, Temporal lobe epilepsy and migraine.
B. Peripheral which involve the vestibular end organs and their 1
st
order neuron (i.e.
the vestibular nerve)
85% of all cases of vertigo.
2
Peripheral vestibular disorders
1. Meniere's disease ( Endolymphatic hydrops)
It is a disorder of the inner ear where the endolymphatic system is distended by
endolymph. It is characterized by (1) Vertigo (2) SNHL and (3) Tinnitus.
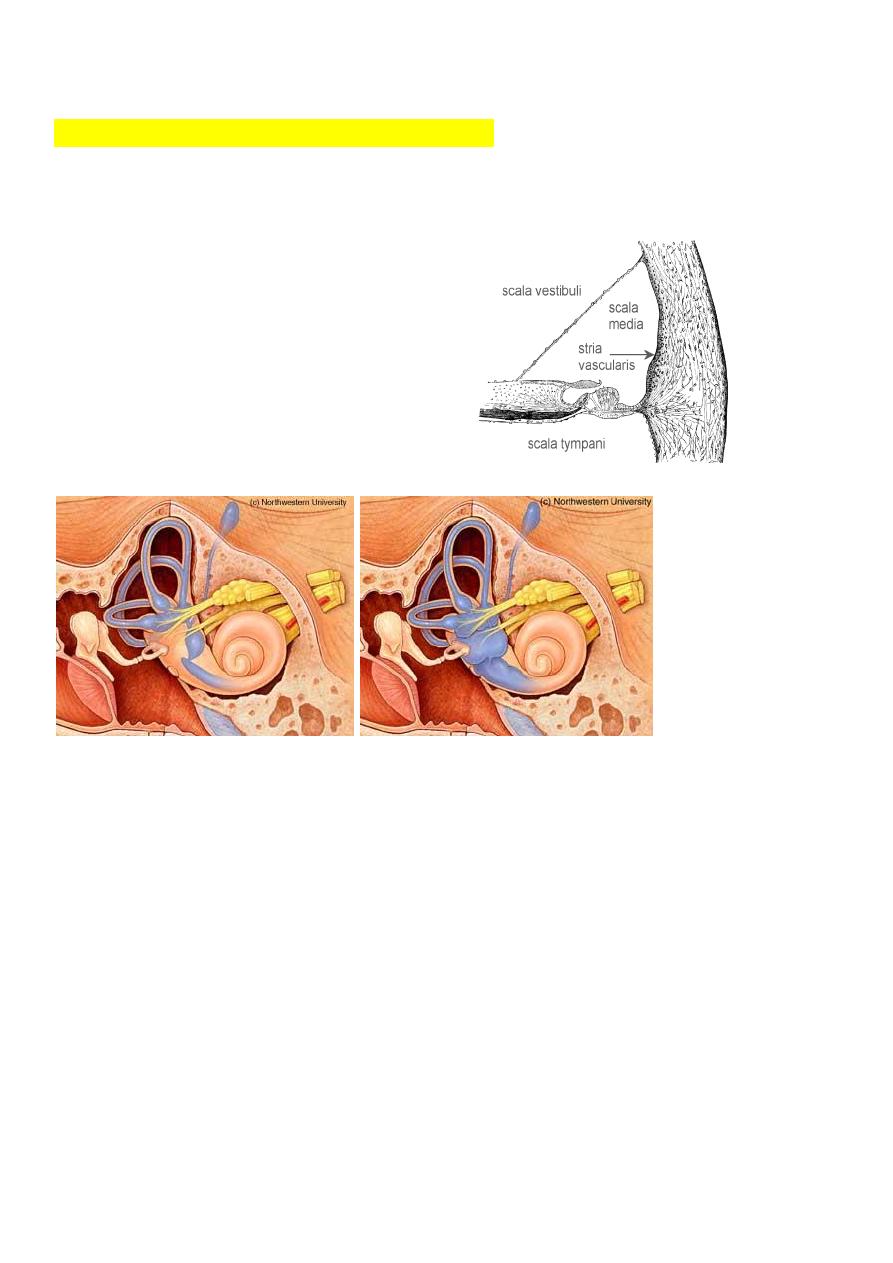
Pathology:
The disease can result either from
increased production of endolymph or its
faulty absorption or both. Normally, the
endolymph is secreted by stria vascularis,
fills the membranous labyrinth and is
absorbed through the endolymphatic sac.
Normal endolymphatic system Endolymphatic hydrops
Aetiology:
The exact cause of Meniere's disease is not yet known. Various theories have been
postulated:
1. Defective absorption by endolymphatic sac; due to ischemia of sac.
2. Vasomotor disturbance.
3. Allergy.
4. Sodium and water retention.
5. Hypothyroidism.
6. Autoimmune and viral aetiology.
3
Clinical features
Age: commonly between 35-60 years.
Sex: no gender bias but some studies states that males are affected more than females.
Usually the disease start unilateral but the other ear may be affected after a few years.
Cardinal symptoms of Meniere's disease are: (1) Episodic vertigo, (2) fluctuating hearing
loss, (3) Tinnitus and (4) sense of fullness or pressure in the involved ear.
Remission is typical of the disease and may vary from a few weeks to several years. The
suddenness of the attack is one of the most characteristic features, though some patients
get warning of attack by change in their tinnitus or a fullness sensation in the ear (aura).
1- Vertigo:
Sudden onset usually without warning.
Last for few hours.
Associated with vomiting, nystagmus, sweating and bradycardia.
The patient may fall and injure himself, BUT he has normal level of consciousness.
2- Hearing loss: it is SNHL and may be during or just after the attack. In the early stages
of the disease the hearing return to normal, but as the attacks become more
frequent, the hearing deteriorates and finally, complete loss of hearing results in the
affected ear.
3- Tinnitus: referred to the affected ear, precedes or accompany the vertigo.
Examination: between the attacks, clinical examination may be completely normal. During
the attacks, the patient is disoriented, unable to stand and usually lie down with: (1)
Nystagmus (2) normal Otoscopy (3) Tuning fork examination SNHL.
Investigation:
1. Audiological (PTA): SNHL.
2. Vestibular (Caloric test): canal paresis in the affected ear
Treatment
I.
Medical
During the acute attack
1. Complete bed rest.
2. Antihistamine & labyrinthine sedatives: prochlorperazine (stemetil) and cinnarzine
(stugeron).
3. Anxiolytics: IV diazepam.
II.
Surgical:
a. Endolymphatic sac decompression or shunt.
b. Vestibular nerve section.
4
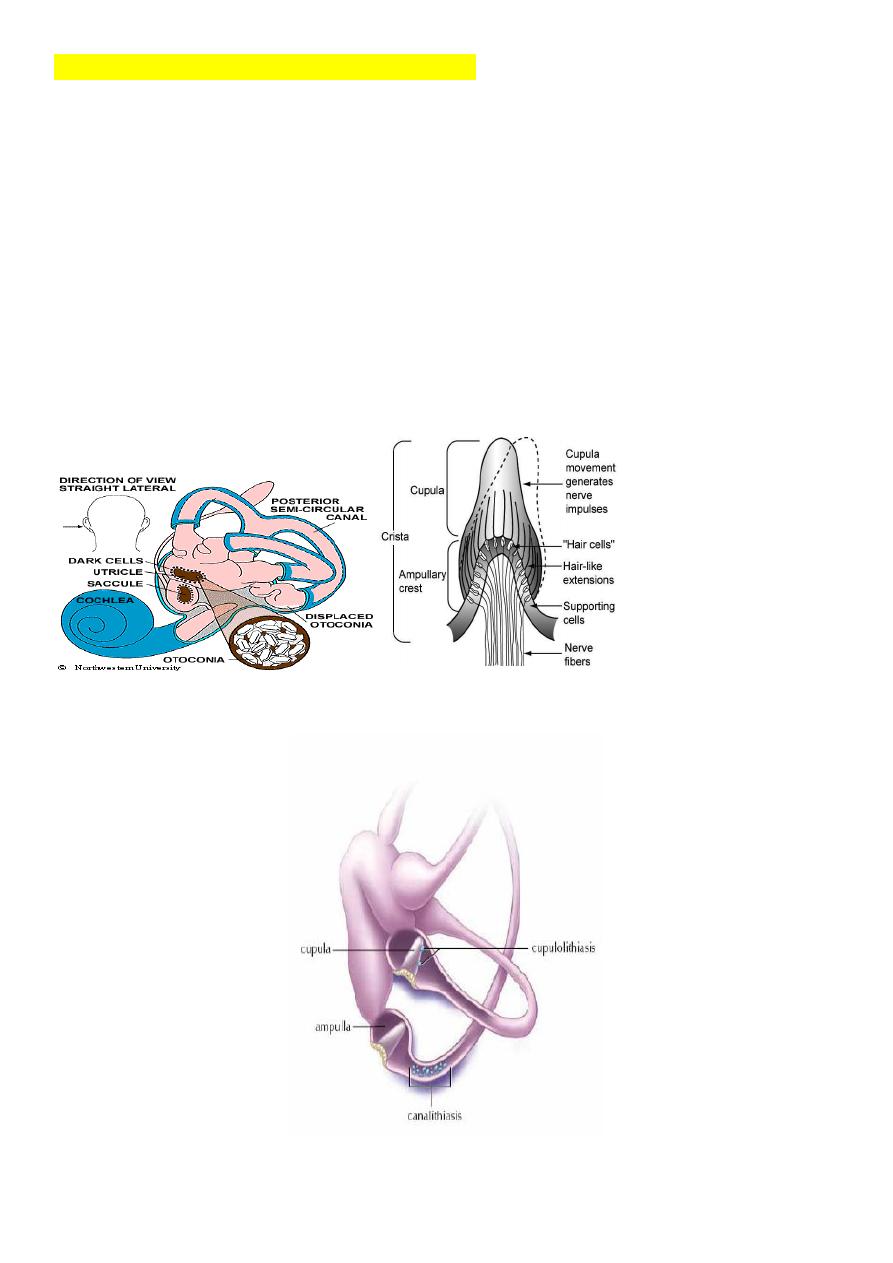
2. Benign Paroxysmal Positional Vertigo ( BPPV)
Recurrent Paroxysmal short lived attacks of vertigo initiated by certain critical positions of
the head. There are no other aural symptoms.
Aetiology
1. Idiopathic.
2. Head injury.
3. Viral infection.
4. Aging process.
Pathology
The disease is thought to be due to displacement of otoliths (calcium carbonate particles)
from the utricle and saccule to the capula of the semicircular canal.

5
Clinical picture
1. Brief attacks of vertigo when the patient put his head in the critical position. This
vertigo may be accompanied by a slight feeling of dizziness.
2. Absence of aural symptoms: hearing is normal and there is no tinnitus.
Examination
1. Positional nystagmus which is elicited by performing Hallpike maneuvers (see lecture
2). The classical features of BPPV are:
a. A latent period of 5-10 sec. followed by rotatory nystagmus lasting up to 30
seconds.
b. The fast component of the nystagmus is directed towards the undermost ear.
c. The nystagmus fatigue rapidly.
2. Normal Otoscopy and audiometry.
Investigation
Caloric test: Normal.
Treatment
I.
Medical:
1. Reassurance and avoidance of the provocating position.
2. Antivertigo drugs: prochlorperazine (stemetil), Cinnarzine (stugeron) and Betahistine
(Serc).
II.
Surgical:
Posterior semicircular canal denervation.
Prognosis
There is normal tendency for spontaneous cure, which may be delayed for several months.
In Central (Malignant) Positional Vertigo, the nystagmus is caused by lesions of the
brainstem or posterior fossa e.g. multiple sclerosis, metastatic lesions and vascular
disorders. Here there is no latent period; the nystagmus persists as long as the head is
maintained in the provocating position. The nystagmus is not fatigable and there is little or
no vertigo. Frequently, there are other associated signs.
3. Vestibular Neuronitis
This condition is characterized by a severe vertigo of sudden onset without deafness or
tinnitus and with no sign of neurological involvement.
Aetiology
The condition is thought to result from a selective inflammation of the vestibular nerve,
presumably of viral origin following a vague URTI.
6
Clinical picture
The onset of symptoms is preceded a week or 10 days earlier by a sore throat, acute
sinusitis or other URTI.
1. Vertigo which can last several days before a gradual recovery begins.
2. Nausea and vomiting.
3. Absence of aural symptoms: Hearing is normal and there is no tinnitus.
Examination
Spontaneous nystagmus of the vestibular type.
Investigations
Caloric test: canal paresis on the affected side.
Treatment
1. Reassurance and explanation while waiting for recovery to occur by compensation.
2. Antivertigo drugs: prochlorperazine (stemetil) and cinnarzine (stugeron) and
Betahistine ( Betaserc)
Prognosis
Vestibular Neuronitis has no complications and recovery is usual in a few weeks.
4. Labyrinthitis
a. Circumscribed labyrinthitis: is seen in case of unsafe type of CSOM, and fistula
test is positive.
b. Serous labyrinthitis: caused by trauma or infection adjacent to the inner ear
without actual invasion. There is severe vertigo and SNHL. A partial or full
recovery of the inner ear function is possible if treated early.
c. Purulent labyrinthitis: Is a complication of CSOM. There is actual bacterial invasion
of the inner ear with total loss of cochlear and vestibular functionsacute
vestibular failure vertigo + severe nausea and vomiting. Nystagmus is seen to
the opposite side due to destruction of the affected labyrinth.
5. Vestibulotoxic drugs: e.g. Aminoglycosides
6. Head trauma: concussion of labyrinth, completely disrupt the bony labyrinth or
VIII cranial nerve, or cause perilymph fistula.
7. Perilymph fistula:
Causes: complication of ear surgery (stapedectomy), barotrauma, raised intracranial
pressure.
Clinical feature: Intermittent vertigo, fluctuant SNHL, sometimes tinnitus and sense of
fullness in the ear (DDx. Meniere's disease).
8. Vestibular schwannoma (Acoustic neuroma)
Are nerve sheath tumors which arise from Schwann cells covering the superior and inferior
vestibular nerve (cranial nerve VIII). Rarely they originate from the cochlear nerve.

7
Vestibular schwannoma represents 8% of all intracranial tumors and 80% of
cerebellopontine angle tumors.
They are slowly growing tumors which do not infiltrate local tissues or metastasize.
However, as they grow they compress the adjacent tissues.
Aetiology
The cause is unknown although neurofibromatosis type 1 (NF1) and NF2 are associated
with Vestibular schwannoma. Bilateral Vestibular schwannoma are common in NF2.
Clinical picture
The tumor occurs equally in both sexes with wide age incidence, usually between 30 – 60
years.
I.Otological symptoms
1. Progressive unilateral SNHL.
2. Unilateral or asymmetrical tinnitus.
3. Balance disturbance is not often a prominent feature because the slow growth of the
tumor allows central compensation to occur.
II. Facial and trigeminal nerve dysfunction started as the tumor starts to expand. The
patient usually has midface numbness, absent corneal reflex and facial weakness.
III. Further expansion leads to brainstem and cerebellar compression and increase
intracranial pressure.
Investigation
1. Audiological: PTA: Shows asymmetrical SNHL, usually worse in the higher
frequencies. Speech discrimination is poor.
2. Imaging: MRI with gadolinium contrast is the gold standard for the diagnosis. CT scan
may detect large tumors but miss small intracranial tumors.
3. Caloric test: canal paresis in the affected side.
Differential Diagnosis
1. Meningioma.
2. Congenital cholesteatoma.
Treatment
1. Observation if the life expectancy of the patient is shorter than the growth time
required for the vestibular schwannoma to cause neurological symptoms
2. Surgical removal.
3. Stereotatic radiation using cobalt-60 gamma knife system. It is reserved for patients
with surgical risks, elderly and those who refuse surgical removal.

8
How to differentiate between central and peripheral type?
History:
Hx alone will dx 3 out of 4 patients.
1. Timing and duration:
The longer the symptoms last, the more likely it is central
Sudden onset more suggestive of peripheral
Early morning vertigo may be more suggestive of peripheral
2. Provoking Factors:
o Positional changes—usually BPPV (Turning in bed, bending at waist and then
straightening, or extending neck)
o Recent viral illness– acute vestibular neuronitis, acute labyrinthitis.
o Trauma, excessive straining (perilymphatic fistula)
3. Associated symptoms: Hearing loss (usually peripheral cause), Pain (acute otitis
media), Nausea/vomiting (usually less severe in central disease), Neurological
Symptoms: weakness, dysarthria, vision changes, and change in consciousness,
ataxia, and motor/sensory changes (suggestive of central type).
4. History of medications, trauma, toxins, DM, hypertension.
5. Family history: Migraine, CVA risk.
Examination:
1. Otological:
a. TM: Vesicles suggest Ramsey Hunt Syndrome (herpes zoster oticus).
Cholesteatoma (CSOM).
b. Hennebert’s sign: Vertigo caused by pushing on tragus or external auditory
meatus of affected side
perilymphatic fistula
c. Valsalva maneuver: Forced exhalation with mouth and nose closed
again
?perilymphatic fistula or semicircular canal dehiscence.
2. Cardiovascular:
Orthostatic changes (drop of BP by 20 mmHg may suggest dehydration
or autonomic dysfunction), arrhythmias, carotid bruits or other signs of atherosclerosis.
3. Neurological:
a- Cranial nerves palsies and sensorineural hearing loss
b- Nystagmus
Vertical– 80% sensitive for vestibular nuclear or cerebellar lesions
Horizontal– suggests peripheral cause
c- Gait and balance
If peripheral, pt will be able to walk
Central –pt usually will be severely impaired in walking
d- Hallpike maneuvers
