Pathology
Obstructive lung diseasesAsthma :
reversible episode of bronchial spasm result from an exaggerated bronchial constriction response to various stimuli.Clinically manifest by episodic dyspnoea, cough and wheezing. It is of two types:
Extrinsic asthma: in which the attack is initiated by type І hypersensitivity reaction induced by exposure to extrinsic a.g.
Atopic asthma is the most common subtype, occur in the first two decades of life ,have associated history of allergy . Serum IGE level is elevated as well as blood eosinophilic count.
Intrinsic asthma: in which the triggering mechanism are not immune. Several stimuli are include , pulmonary viral infection, cold , exercise & psychological stress. There is no personal or family history of allergic manifestation and serum IGE is normal.
Pathogenesis:
In extrinsic asthma the antigen stimuli the formation of IgE antibody which bind to receptor on the mast cell , on second exposure to the same antigen the later react with the antibody result in degranulation of mast cell & the release of histamine and other mediators which open the junction between the epithelial cell so the a.g. enter the mucosa & activate mast cell and eosinophil which intern release additional mediator.Collectively all these mediator either directly or via neural reflex induce bronchospasm , increase vascular permeability and mucus production responsible for early stage of asthma in addition they recruit additional cell from the blood which responsible for the late stage of asthma , they release mediator responsible for epithelial damage & spasm of SMF.
X: over inflation of the lung; occlusion of the bronchi by thick tenacious mucus plug.
M: the mucus plug contain whorls of shed epithelium (curshman body), numerous eosinophils , and charcoat leyden crystal ( made of eosinophilic protein)The mucosa show marked edema, heavy inf. cell infiltrate (eosino. form 50% + lymphocyte &. Mast cell) increase in number of goblet cell; thicker basement. Submucosa show enlargement of mucus glands and hypertrophy of smooth muscle
Emphysema: permanent enlargement of airspace distal to the terminal bronchiole accompany by destruction of their walls.
Types of emphysema:
Centriacinar emphysema dilatation involve respiratory bronchioles only so normal and emphysematous airspaces are found within the lobule. The lesion more sever in the upper lobes. It is more common in heavy smoker.
Panaciner emphysema: the whole acini is involved (from respiratory bronchiole to the alveoli) and more common in the lower lung zone and in ά1 antitrypsin deficiency.
Distal acinar emphysema: the proximal portion of the acini are normal but the distal part is dominantly involved. The lesion usually occur adjacent to the pleura, lobular connective tissue septa, margin of the lobules. It is more sever in the upper half of the lung.
X : panacinar emphysema the lung is pale voluminous that often obscure the heart. In centrilobular the lungs are deeper pink and less voluminous than panacinar. The upper two third of the lung is more affected.
M: thinning & destruction of the alveolar wall and the adjacent alveoli become confluent creating large airspace.
Clinical feature: dyspnoea is the first symptom which is insidious but progressive , weight loss is a common feature . In patient who have underlying chronic bronchiolitis , cough and wheezing may be the initial symptom with less prominent dyspnoea and they are usually hypoxic and cyanosed called blue bloater due to oedema from congestive heart feature. While if the patient has no associated bronchiolitis dyspnoea is marked sitting forward in hunched over position with marked hyperventilation so oxygenation is adequate and such patient is called pink puffer.
Complication: secondary pulmonary hypertension is usually develop and death occur either due to respiratory failure, or due to right sided heart failure.
Pathogenesis:
Smoking play a major role in the development of emphysema .
Tobacco cause leukocyte infiltration (neutrophils and macrophage) via the chemotactic effect of nicotine (both are regarded the main source of protease enzyme especially elastase which normally counteracted by antiprotease ( so patient with ά1 antitrypsin deficiency will suffer from emphysema due to destruction of the tissue by elastase.
In addition tobacco contain free radicals in excess amount which cause inactivation of antiprotease causing (functional ά1 antitrypsin, deficiency.)
Smoking also enhance macrophage to secret macrophage elastase which not inhibited by ά1 antitrypsin and in addition it can digest this antiprotease.
Chronic bronchitis:
Persistent productive cough for at least 3/12 for at least 3 conservative years. It take several form:Simple chronic bronchitis: patient has productive cough with mucus sputum.
Chronic mucopurulent bronchitis: sputum contain pus.
Chronic asthmatic bronchitis: patient with chronic bronchitis & has intermittent episode of asthma.
Chronic obstructive bronchitis: patient develop chronic outflow obstruction.
Pathogenesis:
The commonest causative agent is cigarette smoking, in addition to other pollutant such as SO2, NO2. these irritants cause bronchial hyper secretion , hyperplasia of mucous gland and formation of mucous secreting goblet cells. Also they cause inflammation with infiltrate by T lymphocyte Macrophage and neutrophils. Secondary bacterial infection usually follow result in maintaining the inflammation and exacerbation of symptoms.
The role of smoke in infection ; it interfere with ciliary movement , damage the bronchial epithelium & inhibit the ability of epithelium & leukcocyte to clear bacteria.
Morphology:
The lining of the bronchi become swollen and hyperemic and cover by mucinous or mucopurulent secretion.
M: bronchitis involve large bronchi which show enlargement of mucous secreting gland, increase in the number of goblet cell with contrast loss of ciliated columnar epithelial & stratified squamous metaplasia is seen. A various mononuclear inflammatory cell together with neutrophils.
While in chronic bronchiolitis: goblet cell metaplasia, inflammation fibrosis in the wall and S.M.F. hypertrophy .
Clinical features :
Cough & sputum may persist indefinitely, however as the patient develop evidence of COPD with outflow obstruction, this is accompanied hypercapnia, hypoxia and cyanosis .
complication it may complicate by pulmonary hypertension and cardiac failure. Recurrent infection and respiratory failure are constant features.
Bronchiactasis:
Permanent dilatation of bronchi and bronchioles proximal to the terminal bronchiole , due to destruction of muscle & elastic supporting tissue result from or associated with ch. necrotizing infection.
The disease is usually secondary to persisting infection or obstruction, characterized by cough with expectoration of large amount of purulent sputum.
Predisposing condition:
bronchial obstruction: cause is tumour . and foreign body and occasionally by impact of mucus as in asthma and ch. bronchitis. The lesion is localize to the obstructed lung segment.
Congenital (hereditary): as in cystic fibrosis, immunodeficiency state and katagener syndrome which is autosomal recessive characterize by bronchiectasis and male sterility.
Necrotizing (suppurtive) pneumonia, particularly with virulent m.o. (Staph. aureus or klebsiella spp) or it may complicate tuberculosis.
Pathogenesis:
2 process play in the pathogenesis of Bronchiectasis:Obstruction.
Ch. persistent infection.
Either of these tow process may come first. Normal clearance mechanism may impair by obstruction so secondary bronchial infection soon develop that cause damage to the wall & accumulation of exudates further distend the wall lead to irreversible dilation Conversely ch. infection in time cause damage to the bronchial wall with fibrosis leading to weakening and dilatation.
Clinical feature:
Sever, persist cough with mucopurulent bad odor sputum which may contain stretch of blood sometime frank haemoptysis occur. Clubbing of the finger may develop .
Pathological appearances:
Grossly : It affect the lower lobes , usually bilateral . the dilated bronchi form cavities of variable size lined by thick fibrous wall . the surrounding lung tissue show consolidation .
Microscopic features :
Suppurative exudates in the lumen . the mucosa show ulceration with squamous metaplasia . the wall of bronchi is heavily infiltrated by chronic
Inflammatory cells . the surrounding alveoli show evidence of consolidation i.e.( accumulation of inflammatory exudates & cells in the alveolar spaces ) .
Complication:
Sever bronchiectasis causes hypercapnia, hypoxia and pulmonary hypertension and rarely causes corpulmonale , metastasic brain abscess , amyliodosis is a rare complication.
Pneumonia syndrome :
Inflammation of the lung :
Predisposing conditions :
1- Defects in innate immunity (complement system & neutrophil) & humeral immunity ( immunoglobulin) .
2- cell-mediated immune defects lead to increased infections with intracellular microbes such as mycobacterium and herpes viruses as well as with microorganisms of very low virulence
3- Several exogenous lifestyle factors interfere with host immune defense mechanisms and facilitate infections as, cigarette smoke .
The histological spectrum of pneumonia syndrome :
1- fibrinopurulent alveolar exudates seen in acute bacterial pneumonias.
2- mononuclear interstitial infiltrates in viral pneumonia .
3-granulomas and cavitations in chronic pneumonias.
Community-acquired acute pneumonias:
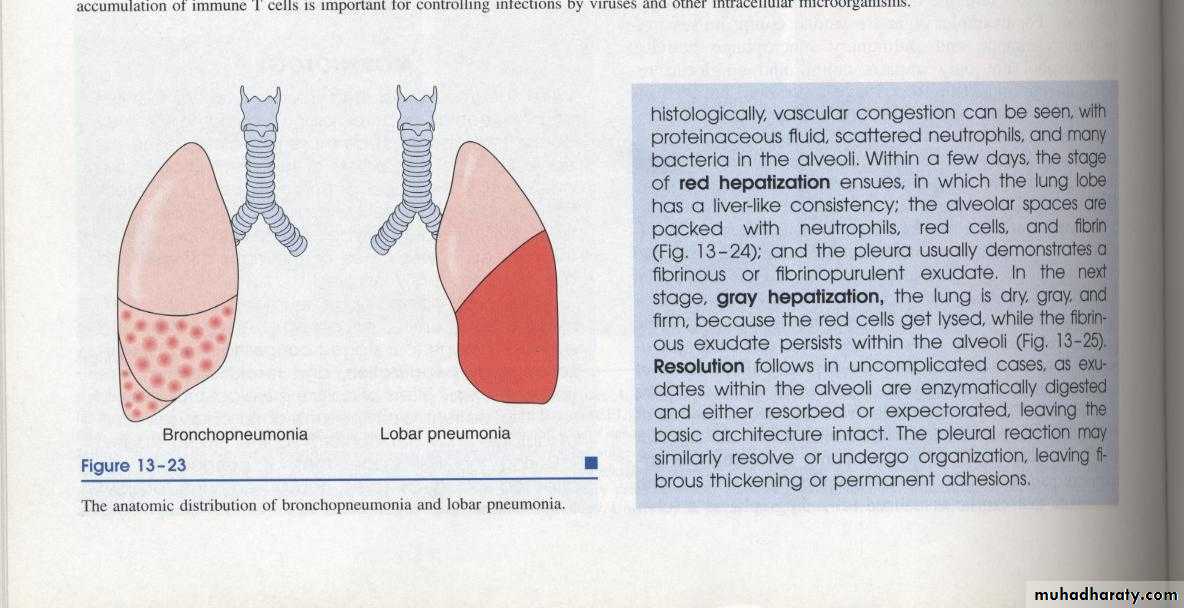
1-lobar pneumonia :part or all of a lobe are homogeneously filled with an exudates. streptococcus pneumonia is responsible for more than 90% of lobar pneumonias.
2-Bronchopneumonia :
a patchy distribution of inflammation that generally involves more than one lobe.Lobar pneumonia
Pneumococcal infections occur in :(1) those with underlying chronic diseases
(2) those with either congenital or acquired immunoglobulin defects
(3) those with decreased or absent spleenic function (e.g., sickle cell disease).
Morphology
It pass into 4 stages but with the use of antibiotic it can arrest at any stage depend on onset of treatment .
1-Stage of congestion : last 1-2 days
X :lobes are heavy & red
Mic :
Congestion of alveolar capillary .
Alveolar space contain inflammatory exudates , red blood cells , bacteria & few neutrophilis .
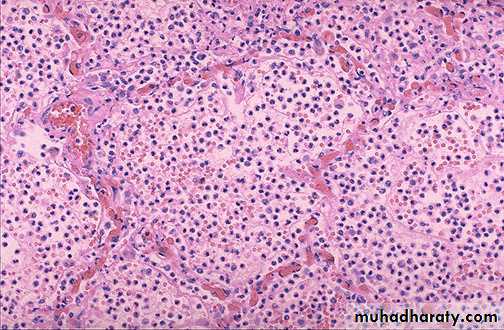
2-Stage of red hepatization ;
X : lobe is heavy , red , firm similar to the liver .Mic : capillary congestion , alveolar space contain red blood cell , neutrophils & fibrin .
Pleural cavity usually show fibrinous or fibrinopurulant exudates .
3- stage of grey hepatization:
X : lobe is grey , firm heavyMic : congestion disappear , alveolar space fill with neutrophils .
Stage of resolution :
The exudates is liquefied by enzymes then it either coughed or absorbed &re-aireation of alveoli take place .
Complication :
Complete healing is usual with proper antibiotics & complication is rare in both types of pneumonia:
(1) organization of the intra alveolar exudates may convert areas of the lung into solid fibrous tissue .
(2) pleural effusion & empyema;
(3)Lung abscess is a rare complication in lobar pneumonia .
(4) bacteremia causing meningitis ,
bronchopneumonia :
foci of inflammatory consolidation are distributed in patches throughout one or several lobes, most frequently bilateral and basal.
Histologically :
* the reaction consist of focal suppurative exudates that fills the bronchi, bronchioles, and adjacent alveolar spaces.
* The intervening areas are normal .
* Pleural involvement is less common than in lobar pneumonia .