THE LIVER
General features.liver weighs 1500g, functions as station between splanchnic & systemic circulations to maintain body’s metabolic homeostasis through -processing dietary carbohydrates, amino acids, lipids, & vitamins -removal of microbes & toxins in splanchnic to systemic circulation -synthesis of plasma proteins -detoxification & excretion of waste products & pollutant xenobiotics
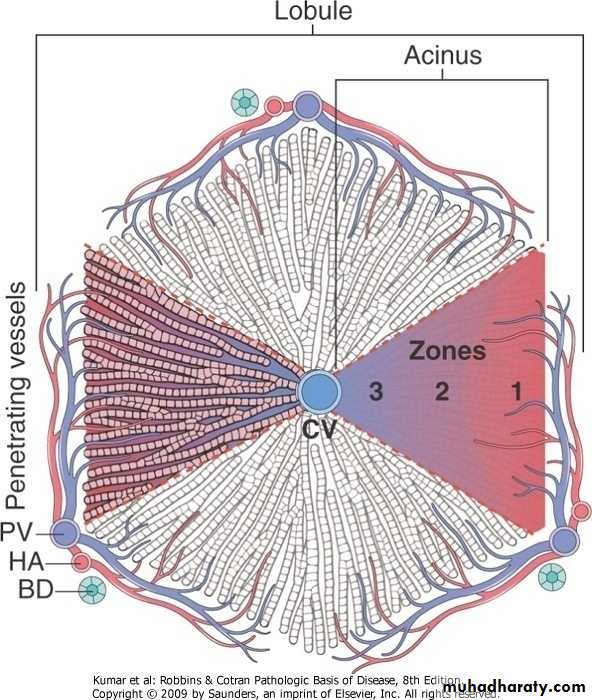
Liver, microarchitecture
General Features of Hepatic Disease
LABORATORY EVALUATION OF LIVER DISEASEmost common.hepatocyte injury, enzymes -(AST, ALT).biliary -substances secreted in bile .(serum bilirubin) -plasma membrane enzymes .(serum alkaline phosphatase).hepatocyte function -(serum albumin, prothrombin time)TYPES OF LIVER DISEASES.metabolic.toxic.microbial.circulatory.neoplastic
PATTERNS OF HEPATIC INJURY• .degeneration & intracellular accumulations
• .cell death
• .inflammation
• .regeneration
• .fibrosis
HEPATIC FAILURE.results from -acute liver injury (massive hepatic necrosis) .drugs (acetaminophen) .toxins (carbon tetrachloride, mushroom) .hepatitis (infection, autoimmune) mechanisms of injury -direct toxic damage -combined toxicity & immune mediated -chronic liver disease (chronic hepatitis> cirrhosis) -hepatic dysfunction without overt necrosis (tetracycline, fatty liver in pregnancy)
.clinical features -jaundice -coagulopathy -hypoalbuminemia>edema -hyperestrogenemia>palmar erythema, hypogonadism, gynecomastia -failure of multiple organ systems -hyperammonemia>encephalopathy .complications -hepatic encephalopathy -hepatorenal syndrome (renal failure) -hepatopulmonary syndrome
CIRRHOSIS
.defined by 3 characteristics-bridging fibrous septae
-parenchymal nodules
-diffuse disruption of architecture
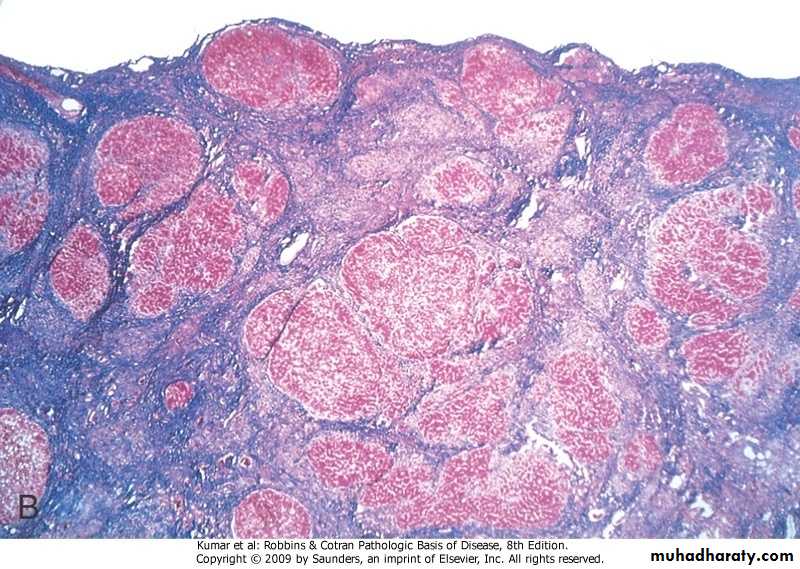
Cirrhosis
Cirrhosis, Masson trichrome
.classification -the best is based on presumed etiology .excessive alcoholic consumption .viral hepatitis .biliary diseases .primary hemochromatosis .Wilson disease .α-1 antitrypsin deficiency .cryptogenic
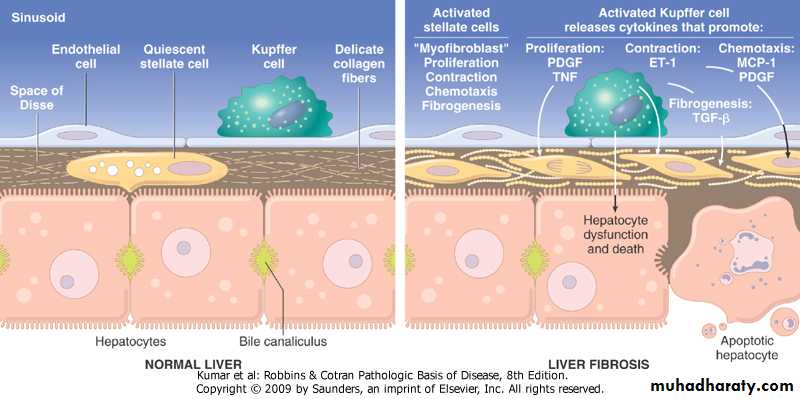
.pathogenesis -death of hepatocytes -extracellular matrix (ECM) deposition (fibrosis) mediated mainly by stellate cells -nodular regeneration of surviving hepatocytes -vascular reorganization
Cirrhosis, pathogenesis
.clinical features
-asymptomatic-non-specific (anorexia, weight loss, weakness)
-hepatic failure
-ultimate cause of death
.progressive liver failure
.portal hypertension
.hepatocellular carcinoma
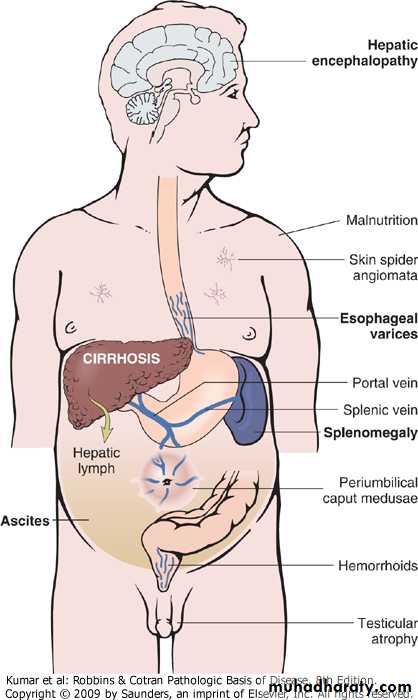
• PORTAL HYPERTENSIION
• .pre-hepatic, (thrombosis, portal vein narrowing, massive splenomegaly).intra-hepatic, (cirrhosis, schistosomiasis,
sarcoidosis, massive fatty change, diseases of portal microcircultion)
.post-hepatic, (severe right-sided heart failure, constrictive pericarditis, hepatic vein outflow obstruction)
.pathophysiology -increased resistance to portal flow at level of sinusoids .contraction of vascular smooth muscle cells & myofibroblasts .disruption of blood flow by scarring & parenchymal nodules -increase in portal venous blood flow .arterial vasodilation in the splanchnic circulation
Clinical consequences of portal hypertension
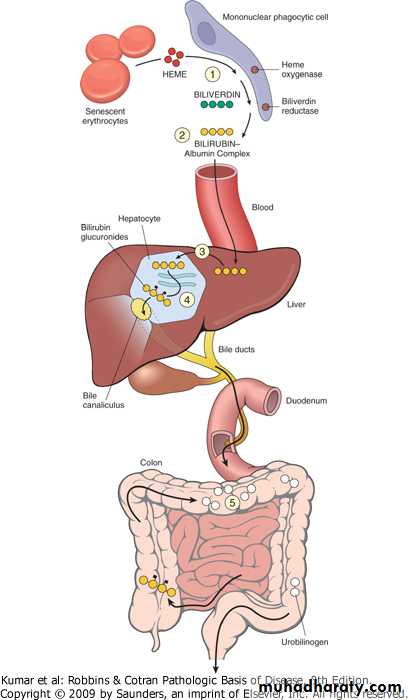
JAUNDICE Jaundice .yellow discoloration of skinIcterus.yellow discoloration of sclera
.pathophysiology of jaundice -disequilibrium between bilirubin production & clearance due to .excessive production of bilirubin (hemolytic anemias, ineffective erythro- poiesis, resorption of blood from internal hemorrhage) .reduced hepatocytes uptake (drugs, genetic) .impaired bilirubin conjugation (genetic, physiologic, diffuse liver disease) .decreased hepatocellular excretion (genetic) .impaired bile flow (obstruction)
Neonatal Jaundice (physiologic jaundice of the newborn) .almost every newborn has transient & mild unconjugated hyperbilirubinemia.exacerbated by breastfeeding, due to presence of bilirubin-deconjugating enzymes in breast milk
Hereditary Hyperbilirubinemias.uncojugated hyperbilirubinemia -Crigler-Najjar syndrome type I (UGT1A1 is completely absent) -Crigler-Najjar syndrome type II (UGT1A1 is greatly reduced) -Gilbert syndrome (UGT1A1 is 30%).conjugated hyperbilirubinemia -Dubin-Johnson syndrome (defect in excretion of bilirubin glucuronides) -Rotor syndrome (defects in uptake & excretion of bilirubin pigments)
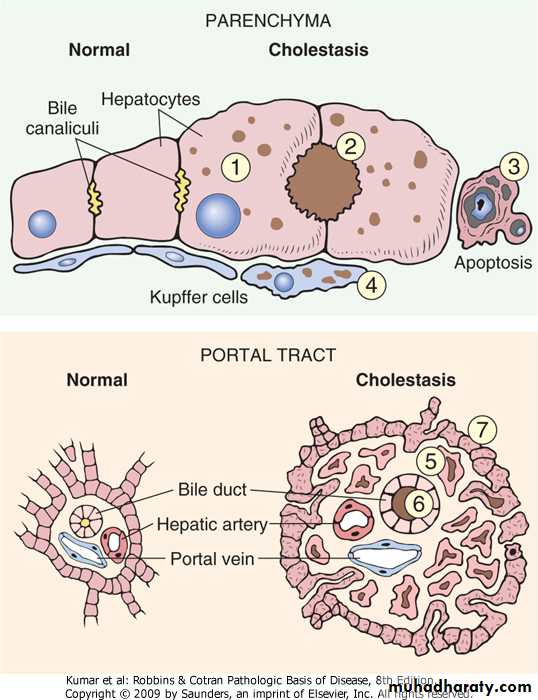
CHOLESTASIS.systemic retention of bilirubin & other solutes eliminated in bile .clinical features (jaundice, pruritis, skin xanthomas, malabsorption syndrome).results from -defects in hepatocyte bile secretion -biliary obstruction .characteristic laboratory finding is elevated serum alkaline phosphatase