
1
|
P a g e
Fifth stage
Gynecology
Lec-1
د. سجى
31/10/2016
Amenorrhoea
Objectives;
To know what is amenorrhea
To understand aetiology and management
To make students able to solve the patient’s problem with amenorrhea
Definition:
• Amenorrhoea is defined as the absence of menstruation.
• It may be classified as either physiological and pathological
physiological amenorrhea :In pregnancy, lactation ,prior to the
onset of puberty and after menopause
Pathological :
• Primary amenorrhoea describes the condition in which girls fail to
develop secondary sexual characteristics by 14 years of age or fail
to menstruate by 16 years of age.
• Secondary amenorrhoea describes the cessation of menstruation
for more than 6 months in a normal female of reproductive age
that is not due to pregnancy
• Oligomenorrhea is defined as menses occurring at intervals longer
than 35 days
2
|
P a g e
Classification:
Reproductive outflow tract disorders.
Ovarian disorders.
Pituitary disorders.
Hypothalamic disorders.

3
|
P a g e
Causes of amenorrhoea:
Reproductive outflow tract disorders
• Asherman's syndrome
• Mullerian agenesis
• Transverse vaginal septum
• Imperforate hymen
• Testicular feminization syndrome
Ovarian disorders
• Anovulation , e.g . polycystic ovarian syndrome
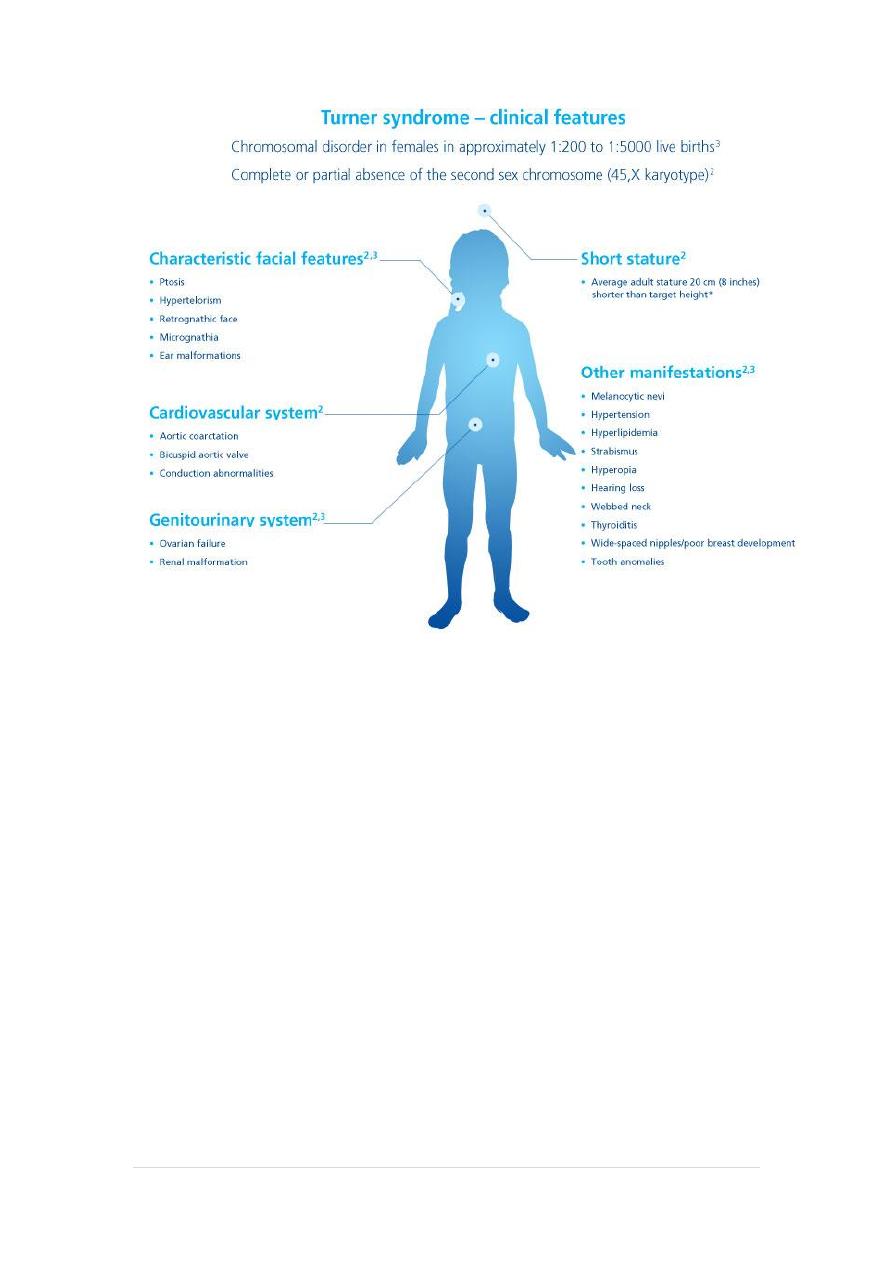
• Gonadal dysgenesis, e.g. Turner's syndrome
• Premature ovarian failure
• Resistant ovary syndrome
Pituitary disorders
• Adenomas such as prolactinoma
• Pituitary necrosis, e.g. Sheehan's syndrome
Hypothalamic malfunctions
• Resulting from excessive exercise
• Resulting from weight loss/anorexia nervosa
• Resulting from stress
• Craniopharyngioma
• Kallman's syndrome
4
|
P a g e
5
|
P a g e
Reproductive outflow tract abnormalities
These may result from abnormal sexual development,
1. Mullerian agenesis
• is a congenital malformation where the Mullerian ducts fail to
develop resulting in an absent uterus and variable
malformations of the vagina..
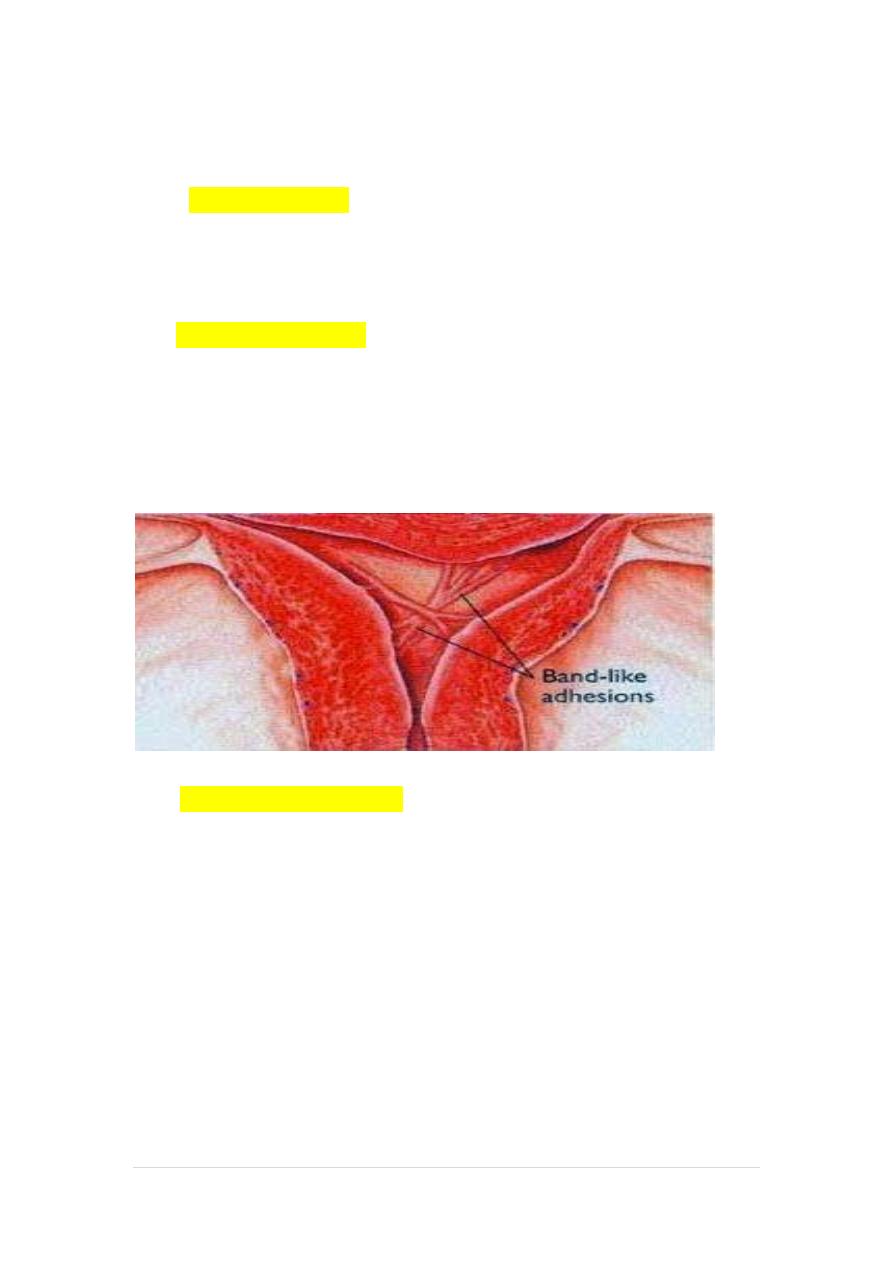
2-Asherman's syndrome:
• This refers to the presence of intrauterine adhesions, which
prevent endometrial proliferation (and thus menstruation).
• The commonest cause of Asherman's syndrome in developed
countries is over-vigorous uterine curettage (e.g. at uterine
evacuation)...
3-Tuberculosis of the uterus :
has similar signs and symptoms with asherman syndrome, and should be
considered in the differential diagnosis in areas where the infection is
endemic
6
|
P a g e
Ovarian disorders
1. Ovarian failure
is the term used to describe the condition in which the stock of
functional primordial follicles is exhausted and normal follicular
development fails to occur despite the pituitary producing
increasing amounts of gonadotrophins (luteinizing hormone
[LH] and follicle-stimulating hormone [FSH]).
2-resistant ovary syndrome
• It has recently become clear that some women present
with symptoms, signs and blood results identical to those
of ovarian failure but that they do in fact have viable
follicles in the ovary.
• These follicles are unresponsive to elevated
gonadotrophin levels, giving rise to the term resistant
ovary syndrome women with the resistant ovary
syndrome may occasionally ovulate and conceive
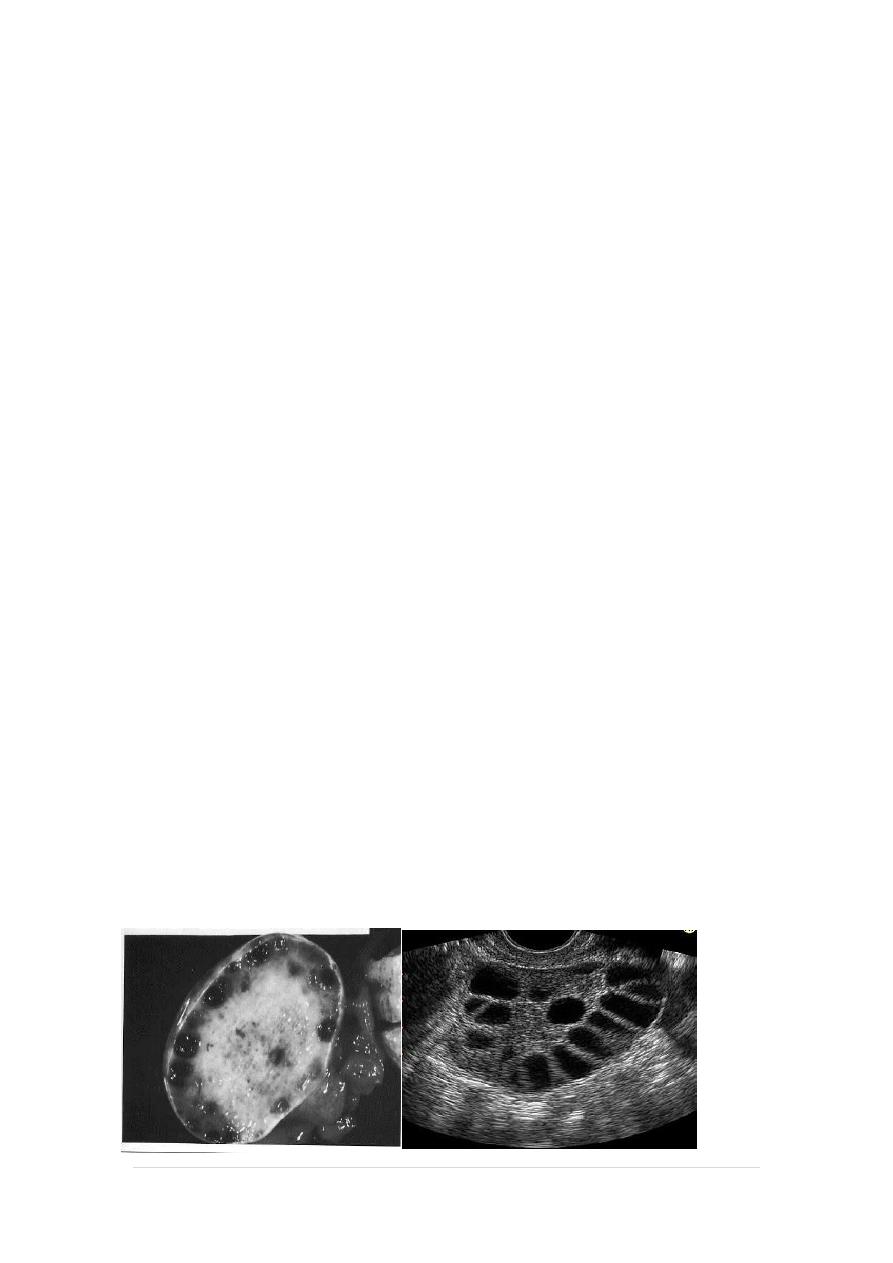
3-polycystic ovary syndrome
• The other common ovarian disorder leading to
anovulation and amenorrhoea is PCOS

7
|
P a g e
Pituitary disorders
1-prolactinoma
• The commonest of these, the prolactinoma, which is
microadenoma secretes prolactin.
• This causes the symptom of galactorrhoea and inhibits
gonadotrophin activity, leading to oligomenorrhoea or
amenorrhoea.
• Prolactinomas normally respond very well to treatment
with bromocriptine or to newer drugs such as cabergoline
• Women with significantly elevated prolactin levels (>
1000 pmol/L) should therefore be further investigated
with computerized tomography (CT) scanning or magnetic
resonance imaging (MRI) to visualize the pituitary.
• Prolactin levels may alternatively be elevated as a side
effect of some drug treatments (e.g. phenothiazines), and
thus is it worth reviewing the drug history in any patient
with hyperprolactinaemia
Hypothalamic disorders
Excessive weight loss (to 15-20 per cent below ideal body weight)
and/or excessive exercise can lead to amenorrhoea by switching off
hypothalamic stimulation of the pituitary (hypogondotrophic
hypogonadism).
Such women will have low (or normal) gonadotrophin levels

8
|
P a g e
Clinical features of oligomenorrhoea/amenorrhoea
A comprehensive history will include:
• developmental history,
• age of onset of menarche,
• presence or absence of cyclical symptoms.t-
• history of chronic illness,
• excessive weight loss/presence of an eating disorder,
• excessive exercise
• history or family history of anosmia,
• menstrual/contraceptive and reproductive history,
• past medical and surgical histories,
• presence of menopausal symptoms,
• current medications,
• family history of premature menopause
• development of any virilizing signs
• or galactorrhoea (milk discharge from breasts),
• psychological history,
• recent stressful events (past or present history of depression or an
eating disorder).

9
|
P a g e
Clinical examination
1. Height:
• an abnormality in appropriate height for age may reflect an
underlying chromosomal disorder (patients with Turner's
syndrome are often short, whereas patients with androgen
insensitivity are often tall).
2. Development of secondary sexual characteristics or any evidence
of abnormal virilization
3. Visual field disturbance or papilloedema may imply a pituitary
lesion
4. Breast examination for presence of secodary sexual characters
and galactorrhea
5. Inspection of external genitalia may suspect imperforated hymen
6. Rectal examination in single ladies may detect abscent uterus
7. Pelvic examination( in married ladies) may detect any pelvic
organs anomalies
8. Also look for evidence of atrophic effects of hypo-oestrogenism
within the lower genital tract

11
|
P a g e
Investigations
Step 1:
͏ Initial hormone tests
• Pregnancy test
• Prolactin
• Thyroid function
• LH and FSH
• Testosterone
͏ Imaging studies
Ultrasound :
• Determine the presence, state and size of ovaries and any
follicular activity .
• Determine the presence and size of uterus
͏ Chromosomal analysis:
• chromosomal analysis and Karyotype should be done in
primary amenorrhea if the diagnosis not clear with
suspicion of chromosomal anomaly.
• In Karyotype A buccal smear and examination of the
polymorphnuclear leucocytes to determine if chromatin
positive (XX) or chromatin negative (XO or XY) and some
time full chromosomal analysis may be need
͏ Progesterone withdrawal test
• This involves giving a progesterone (such as
medroxyprogesterone acetate 10 mg) for 5 days, and
then stopping.
• If the outflow tract (uterus a d vagina) is normal, and
there is sufficient endogenous oestrogen to induce
endometrial proliferation, progesterone will decidualize
the endometrium.
• On withdrawing the progesterone, the decidualized
endometrium will break down, and menstruation will
ensue.
11
|
P a g e
Step 2
• If the patient does not bleed in response to progesterone,
she should be given orally active oestrogen (e.g.
oestradiol 2 mg) for 21 days, followed by progesterone as
above.
• If the patient still fails to bleed in response to this
treatment, the diagnosis is one of an outflow tract
abnormality.
• If bleeding does occur in response to sequential
oestrogen and progesterone, this indicates the problem is
in the hypothalamo-pitl!itaryovarian axis
Step 3
• Having excluded an outflow tract disorder, measurement
of the LH and FSH levels should be repeated.
• Ideally, this should be done 6 weeks after the initial tests
were performed, and 2 weeks after administration of
either oestrogen or progesteroneI.
• Elevated LH and FS H levels (> 40 lUlL and 30 lUlL,
respectively) on two or more occasions at least 6 weeks
apart and in the absence of menstruation suggest ovarian
failure.
• If LH and FSH levels are not elevated, and the above
scheme of investigation has been followed, the disorder
can be reliably localized to the hypothalamus.
• This is commonly due to stress or weight loss (including
weight loss due to anorexia nervosa), but may also be
seen in severe systemic illness

12
|
P a g e
Laproscopy:
• Laproscopy rarely used to assess pelvic organ.
• It is useful in:
a. cases which there is doubt about the nature of the
gonads.
b. cases where ovarian biopsy is needed to determine
presence of primordial oocytes
Treatment
• The treatment of amenorrhoea depends somewhat on
the cause
• In women in whom endogenous oestrogen levels are low
(e.g. ovarian failure or hypogonadotrophic
hypogonadism), oestrogen -and progesterone
replacement (e.g. in the form of HRT)
• In Cases of Turner's syndrome Induce breast development
by very gradually increasing oestrogen doses then change
to definitive treatment of hormone replacement therapy
(estrogen and progestrone). They have no hope to
achieve pregnancy.
• In hypogonadotrophic hypogonadism who seek fertility
will need therapy with either human menopausal
gonadotrophin injection or gonadotrophin releasing
hormone (GnRH).
13
|
P a g e
androgen insensitivity
* Excision of gonads as this gonad is a testis and there is a
malignant potential in about 30% of cases
*Creation of neovagina to permit sexual
intercourse.
*Treatment with oestrogen to augment breast development
and prevent osteoporosis
Imperforate hymen
The imperforate hymen may at two ages
It may present in:
1-Early childhood :When the infant presents with a bulging
hymen behind which is a mucocele, the vagina expanded by
vaginal secretions of mucus.
2-At puberty:The very distensible features of vagina allow quite
large quantities of blood to collect in some cases.
This situation is known as haematocolpos.
When some blood does accumulate within the uterine cavity it
is known as a haematometra

14
|
P a g e
Clinical assessment:
• A pubertal girl complains of intermittent cyclical abdominal pain.
• The pain is due to dysmenorrhoea associated with the
accumulation of menstrual blood within the vagina.
• As the mass enlarges there may be associated difficulty with
micturition and defaecation and even associated with retension of
urine in some cases.
Examination:
• The patient has normal height & normal secondary sexual
characteristic
• Occasionally there is abdominal mass.
• Pelvic examination by inspection of external genitalia showed a
tense bulging bluish membrane (which is the hymen) closing the
introitus.
• Ultrasound reveals blood collection in the vagina and uterus.
Treatment
• After explanation of the condition and obtaining parents
consent,a cruciate incision (+) in the hymen allows drainage of the
retained menstrual blood with good antibiotic cover to prevent
infection.
• From medico-legal point of view, the girl must be given a report
confirm that the hymen was opened by surgical operation as
treatment
15
|
P a g e
Medical treatment:
Anovulation:
In patient desire pregnancy, ovulation induction agents as clomiphene or
gonadotrophins may be used.
In patient not desire pregnancy can use combined oral contraceptive
pills or cyclic progestogens
Premature menopause
is managed as menopause use hormone replacement therapy (HRT) to
prevent osteoporosis
hyperprolactinemia
Medical
• Use Dopamine agonists (Bromocriptine) 2.5mg daily for three days
then 2.5 mg twice a day for six months.
• It should be stopped if pregnancy occurs.
• Cycle retain once Prolactin levels are retain normal.
• Surgical treatment should be performed for patients with
significant visual field defects or symptoms that can not be
relieved by medical therapy
Surgical treatment:
Some pituitary and hypothalamic tumors may require surgery and, in
some cases, radiation.
Asherman's syndrome requires hysteroscopic lysis of the intrauterine
Adhesions
www.muhadharaty.com/lecture/13667
