Interstitial Lung Disease TUCOMInternal Medicine 4th class Dr. Hasan.I.Sultan
Interstitial Lung Disease (ILD)ILD is a heterogeneous group of pulmonary diseases characterized by diffuse lung injury and inflammation that frequently progresses to irreversible fibrosis and severely compromised gas exchange.
classified together because of similar clinical, radiographic, physiologic, or pathologic manifestations.
Features common to ILD
Clinical presentationCough: usually dry, persistent and distressing
Breathlessness: usually slowly progressive, insidious onset.
Examination findings
Crackles: typically bilateral and basal
Clubbing: common in idiopathic pulmonary fibrosis
Central cyanosis and signs of right heart failure in advanced disease
Radiology
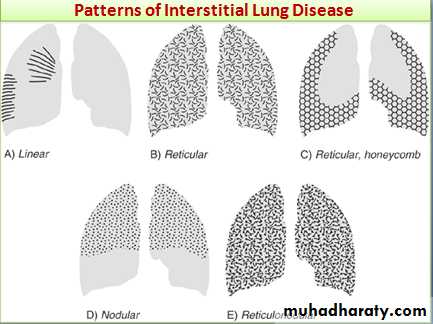
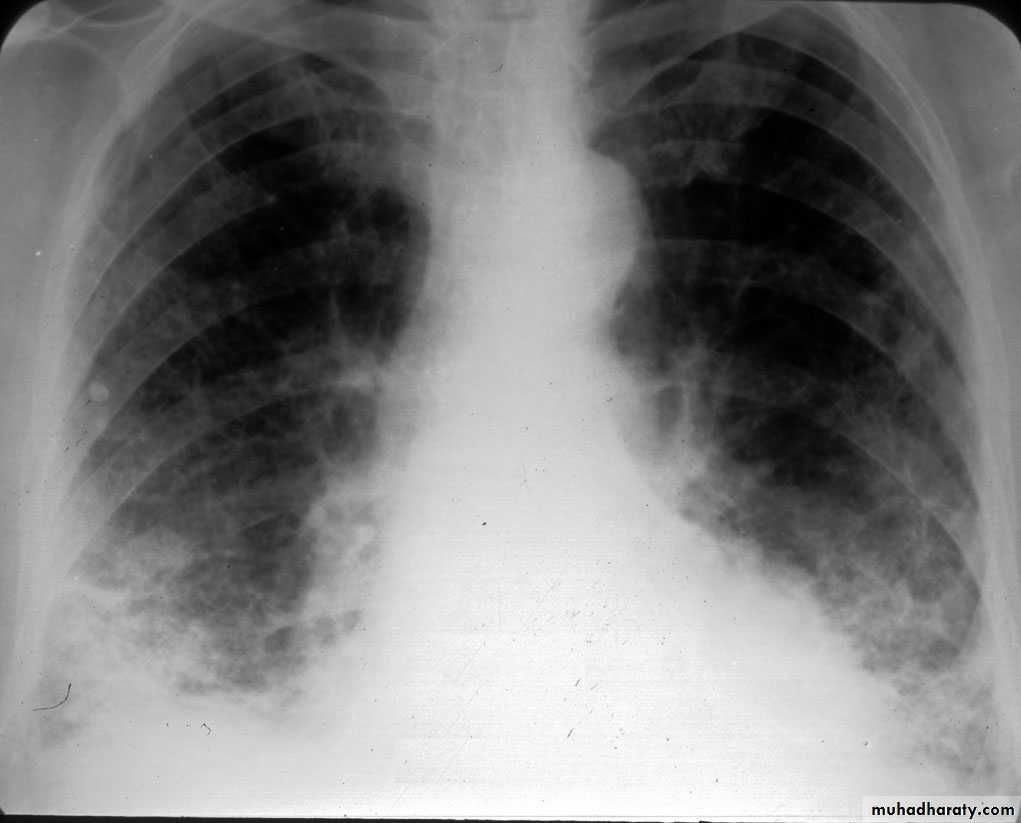
Chest X-ray: typically small lung volumes with reticulonodular shadowing
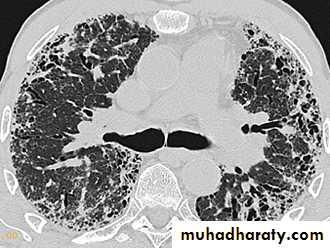
HRCT: reticulonodular shadowing in early stage and honeycomb cysts and traction bronchiectasis in advance stage.
Pulmonary function
Typically restrictive ventilatory defect with
reduced lung volumes and impaired gas transfer.
results of PFT in restrictive lung disease:
Both forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) are reduced, however, the decline in FVC is more than that of FEV1, resulting in FEV1/FVC ratio higher than 80%.
Both total lung capacity and lung volumes are reduced.
Reduce diffusing capacity of the lung: decrease the transfer of gas from air to the lung by using carbon monoxide (CO), (DLCO).
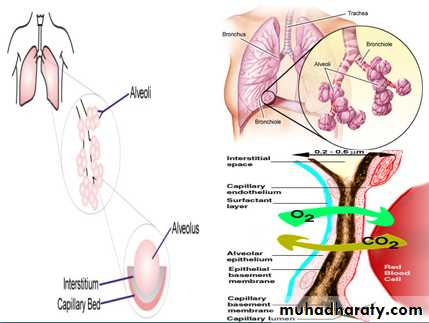
The Lung Interstitium
The interstitial space is defined as continuum of loose connective tissue throughout the lung. It concerns with alveolar epithelium, pulmonary capillary endothelium, basement membrane, perivascular and perilymphatic tissues, subpleural and interlobular septae.The interstitium of the lung is not normally visible radiographically; it becomes visible only when disease (e.g. edema, fibrosis, tumor) increases its volume and attenuation.
Classification
• ILD of unknown causes; Sarcoidosis and idiopathic pulmonary Fibrosis (fibrosing alveolitis)• ILD due to organic dusts exposure;
• a-Hypersensitivity pneumonitis (extrinsic allergic alveolitis); Farmer's lung, Bird fancier's lung, Malt worker's lung, Cheese worker's lung, Maple bark stripper's lung.
• b-Byssinosis; is acute bronchiolitis due to cotton dust inhalation.
• c-Inhalation ('humidifier') fever.
3- ILD due to inhalation of inorganic dusts;
a-Coal worker's pneumoconiosis; inhalation of coal dust .
b-Silicosis; inhalation of silica dust.
c-Asbestosis; due to inhalation of asbestos fibers.
d-Berylliosis; due to inhalation Beryllium.
4- ILD due to systemic inflammatory diseases; due to connective tissue disorders; Rheumatoid disease, systemic lupus erythematosus, systemic sclerosis.
5- ILD due to irradiation.
Idiopathic pulmonary fibrosis
IPF is defined as a progressive fibrosing interstitial pneumonia of unknown cause, occurring in adults and associated with the histological or radiological pattern of usual interstitial pneumonia (UIP). Previously known as cryptogenic fibrosing alveolitisThere is some role of viral exposure e.g. EBV, occupational dust e.g. metal or wood, drugs e.g. antidepressant or GERD. There is a strong association with cigarette smoking.
Clinical features; usually patients more than 50 yrs, progressive breathlessness and a non-productive cough.
Arthralgia may be reported. Finger clubbing and late inspiratory crackles at lung bases. advanced cases central cyanosis and cor pulmnale.
Investigations
Rheumatoid factor and antinuclear factor can be detected in 30-50% of patients. (ESR) is elevated in most cases.Pulmonary function tests show a restrictive defect with reduced lung volumes and gas transfer.
Abnormal chest X-ray at presentation with lower zone bi-basal reticular and reticulonodular opacities. 'honeycomb' appearance in advanced disease.
HRCT may be diagnostic, demonstrating a patchy, predominantly peripheral, subpleural and basal reticular pattern with subpleural cysts (honeycombing).
BAL (bronchoalveolar lavage) and transbronchial biopsy may be used to exclude alternative diagnoses. Not require in typical clinical features and HRCT.
Management
Treatment is difficult. Although the combination of prednisolone, azathioprine and N-acetylcysteine in large studies suggest that it is mostly ineffective.Treat gastro-oesophageal reflux, pulmonary hypertension and supplementation of oxygen.
Lung transplantation should be considered in young patients with advanced disease.
A median survival of 3 years.
sarcoidosis
Sarcoidosis is a multisystemic granulomatous disorder of unknown aetiology. seen in colder parts of Northern Europe. Characterized by non-caseating granuloma. Over 90% of cases affect the lungs.• Berylliosis
Similar clinical and radiological features to sarcoidosis, charactrized by lung granulomas and interstitial fibrosis.
occur in persons working in aircraft, atomic energy and electronics industries.
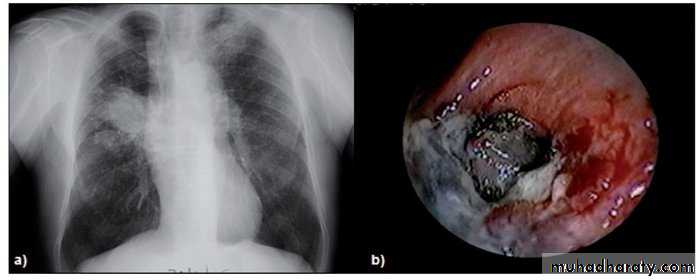
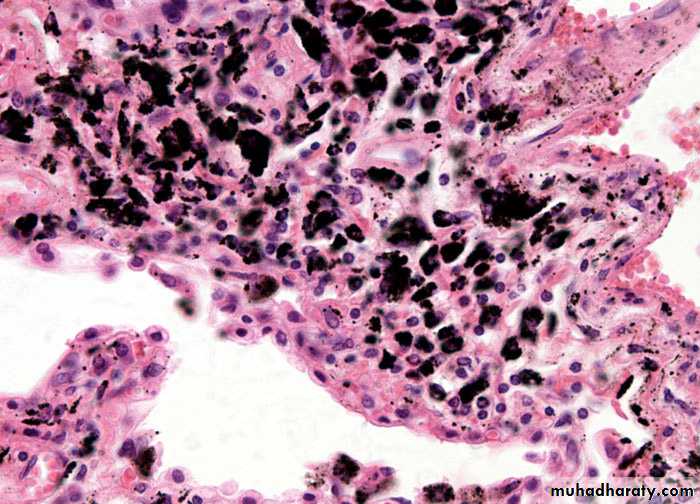
Coal worker's pneumoconiosis
Pulmonary fibrosis caused by prolonged inhalation of coal dust. Which divided into;1-Simple coal worker's pneumoconiosis (SCWP); scattered discrete fibrotic lesions, does not cause pulmonary function abnormalities or progress following cessation of exposure.
2-Complicated pneumoconiosis; large dense masses appear mainly in the upper lobes (also known as progressive massive fibrosis, PMF). Presented as cough, production of sputum, that may be black (melanoptysis) and breathlessness. Respiratory failure after cessation of exposure and right ventricular failure.
3-Caplan's syndrome describes the coexistence of rheumatoid arthritis and rounded fibrotic nodules 0.5-5 cm in diameter.
Coal mining
Coal dustSimple coal worker's pneumoconiosis
Complicated pneumoconiosisCaplan's syndrome
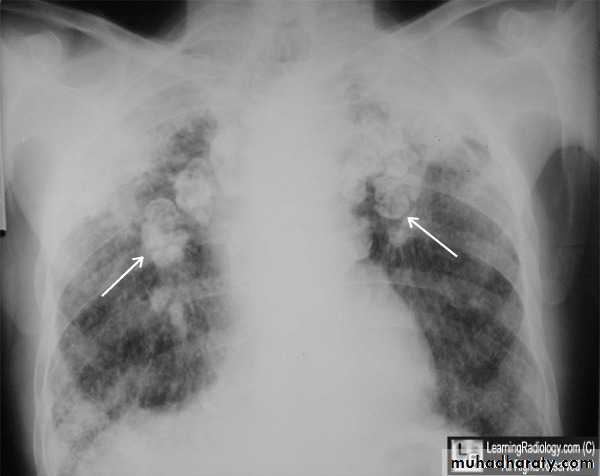
Silicosis
Silicosis results from the inhalation of crystalline or free silica.Silica is highly fibrogenic and the disease is usually progressive (even when exposure ceases).
The clinical and radiological features are similar to those of coal worker's pneumoconiosis, with multiple well circumscribed 3–5-mm nodular opacities, predominantly in the mid- and upper zones
Enlargment of the hilar glands with an 'egg-shell' pattern of calcification is characterestic.
Silicosis are at increased risk of tuberculosis (silicotuberculosis), lung cancer and COPD.
metal grinding
stone dressing
pottery
Asbestosis
Is a diffuse interstitial fibrosis of the lungs that may or may not be associated with pleural fibrosis due to exposure to fibrous mineral asbestos.Requires substantial exposure over several years
Risk factor for carcinoma of the lung and larynx
Exertional breathlessness and fine, late inspiratory crackles over the lower zones and digital clubbing.
Chest X-ray; Shows bi-basal reticular nodular shadowing and asbestos-related pleural disease is usually present. HRCT scanning is more sensitive.
Pulmonary function tests; Typically show a restrictive defect with decreased lung volumes and reduced gas transfer factor.
Asbestos bodies may be identified in sputum or BAL and confirm asbestos exposure.
Asbestos dust
Demolition
Ship breaking
manufacture of fireproof insulating materials and brake-pads
Pipe Insulation
Management
No specific treatment is availablePrevention of occupational lung disease:
• Limit exposure to safe level with specific respiratory protection
• Medical screening for early evidence of disease
• Stop smoking
• Change the job of patient because respiratory symptoms related to occupation
• Patient develop work related disability must be established in worker’s compensation systems.