Introduction to rheumatology
JOINTSBones are linked by joints. There are three main subtypes.
Fibrous joints: characterized by limited movement like skull sutures.
Fibrocartilage joints: These joints comprise a simple bridge of fibrous or fibrocartilage tissue joining two bones together where there is little requirement for movement. The intervertebral disc is a special type of fibrocartilage joint in which an amorphous area termed the nucleus pulposus lies in the centre of bridge.
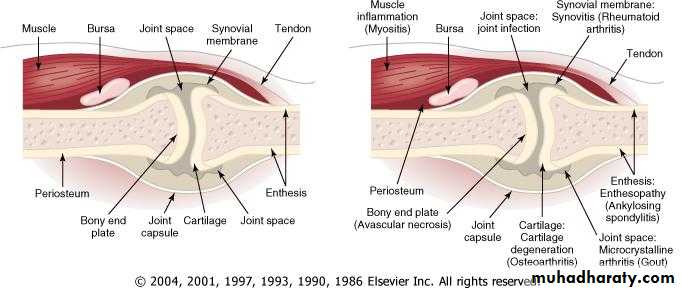
Synovial joints: Synovial joints are more complex structures containing several cell types and are found where a wide range of movement is required. In synovial joints the bone ends are covered by articular cartilage. This is an avascular tissue consisting of chondrocytes embedded in a meshwork of type II collagen fibrils that extend through a hydrated 'gel' of proteoglycan molecules. For example, the knee joint.
Major Symptoms in Joint Disorders
PainStiffness
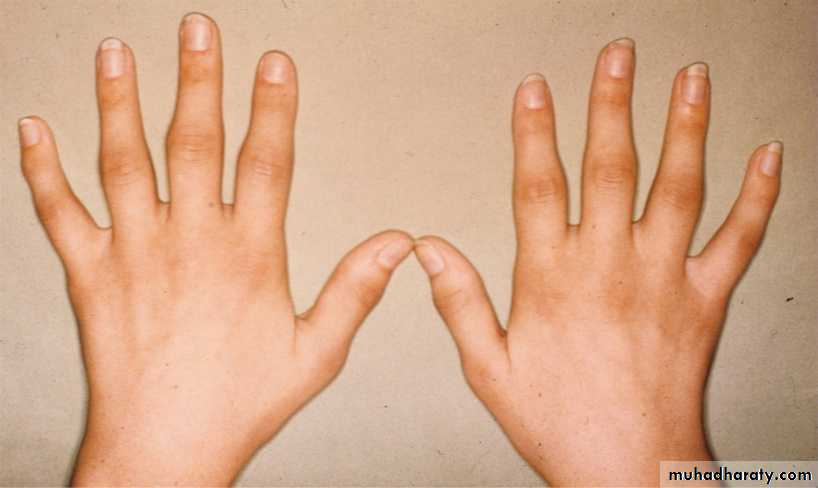
Joint swelling and deformity
Functional impairments
Systemic manifestations
Extra-articular features
IMPORTANT MSK SYMPTOMS
Pain
Usage pain-worse on use, relieved by rest (mechanical strain, damage)
Rest pain-worse after rest, improved by movement (inflammation)
Night or 'bone' pain-mostly at movement (bone origin)
Stiffness
Subjective feeling of inability to move freely after rest.
Duration and severity or early morning and inactivity stiffness that can be 'worn off' suggest degree of inflammation.
Weakness
Consider primary or secondary muscle abnormality.
Swelling (Fluid, soft tissue, bone)
Deformity (Joint, bone)
Non-specific symptoms of systemic illness (Reflecting acute phase reaction)
Weight loss, ± reduction in appetite
Fatigability, poor concentration
Sweats and chills, particularly at night
Feeling ill.
Arthralgia is pain in one or more of your joints. The pain may be described as sharp, dull, stabbing, burning or throbbing, and may range in intensity from mild to severe.
Arthritis is a joint disorder featuring inflammation. A joint is an area of the body where two different bones meet. A joint functions to move the body parts connected by its bones. Arthritis literally means inflammation of one or more joints
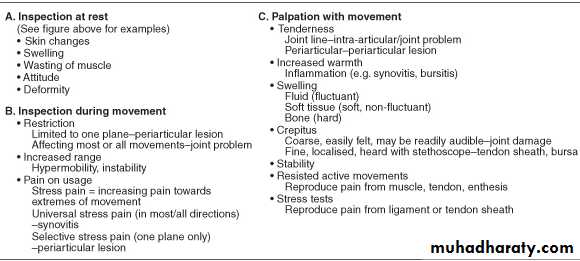
Examination:
Classification of Joint Disorders
R.A. / sero-ve spondarthritis / SLE / …Inflammatory / autoimmune disorders
Disc prolapse / meniscus tear …etc
Mechanical disorders
Septic / T.B. / Brucella / gonococcal … etc
Infective
Gout & pseudogout
Crystal induced
Traumatic joint disorders
Tendinitis / bursitis / capsulitis / epicondylitis / carpal tunnel … etc
Periarthritis
Joint Profile in Various Disorders
R.A.
Chronic symmetrical small & large joints
O.A.
Psoriatic Arthritis
Gout
Distal inter-phalangeal joints
O.A.
Cervical & lumbar spine
Thumb base
Knees & hips
No systemic or inflammatory features
Sero-ve spondarthritis (reactive arthritis)
Asymmetrical large joints arthritis + reactive evidence (past diarrhea, urethritic …)
Ankylosing spondylitis & allied conditions
Sacro iliac + lumbar spine + inflammatory / systemic featuresTraumatic
Infective arthritis
Crystal arthritis
Acute flare of chronic disease
Mono-articular onset of a systemic disease
Intra-articular bleeding
Acute mono-arthritis specially knee or hip
Clinical pointers to isolated periarthritis
Typical clinical pattern e.g. carpal tunnel syndrome, plantar fasciitis & tennis elbow.
Good general health.
Tenderness outside joint margin.
Swelling is absent or outside the joint.
Examples: plantar fasciitis, subdeltoid bursitis, elbow epicondylitis.
Joint redness
Acute gout
Acute septic arthritis
Acute psoriatic arthritis
Flare up of DIP O.A. (Heberden’s nods)
Inflamed overlying skin
Migratory Arthritis:
Rheumatic fever
Typical (classical) pattern; arthritis does not remain in a single joint more than 7 days.
Gonococcal arthritis
Viral arthritis
SLE
Idiopathic juvenile arthritis
Poly articular gout
Lyme disease
Acute reactive arthritis
others
Migratory element
Acute Mono-arthritis History
Monoarticular presentation of oligo\poly- arthritis:
R.A
Erythema nodosum
Juvenile idiopathic arthritis
Reactive, psoriatic or other seronegative spondarthritis
Causes of acute monoarthritis (in a previously normal joint):
Septic arthritis
Crystal synovitis
Trauma
Haemarthrosis
Foreign body reaction
Chronic Monoarthritis
Not rare in IraqT.B. arthritis
Early stages
Spondarthritis
Pauci-articular JA
At early presentationR.A. & other chronic inflammatory joint disease
Osteoarthritis
Mechanical disorders (“secondary arthritis”)
Chronic polyarthritis: selected causesRheumatoid arthritis and other immune related disorders such as juvenile rheumatoid arthritis , spondylarthropathies , systemic lupus and other connective tissue diseases .
Generlized osteoarthritis .
Gout .
Pseudogout .
Sarcoidosis .
Investigations
Blood & Urine tests in Rheumatology
Inflammatory markers (acute phase reactants), e.g. ESR and CRP.
Immunological tests:
Auto antibodies e.g. RF in rheumatoid arthritis , ANA in SLE , … etc
complement and complement components
HLA association e.g. HLA-B27 association with ankylosing spondylitis and other seronegative spondarthritides .
PLAIN RADIOGRAPHY
Soft tissue swelling.
Decreased bone density (osteopenia) or increased bone density (osteosclerosis) which may be localised or generalised
Bone enlargement and deformity
Joint erosion (non-proliferative or proliferative marginal erosion, central erosion)
joint-space narrowing (focal-osteoarthritis; generalised-inflammatory arthritis)
new bone formation (osteophyte, enthesophyte, syndesmophyte) and periosteal reaction
calcification (cartilage-chondrocalcinosis; synovium, capsule, ligament, tendon, muscle, fat, blood vessels, skin) and intra-articular osteochondral bodies
Erosions:
Osteoporosis / osteomalacia
OsteopeniaR.A.
Marginal wide mouth erosion
Gout
Marginal narrow mouth erosion
O.A.
Subchondral cyst
O.A.
Bone proliferation (osteophytes & subchondral sclerosis)
Perthes disease
Avascular necrosis
Non arthritic bone damage
Osteoporosis
Early spondylitis
Compression fracture (osteoporosis or trauma / vertebral collapse (T.B))
Chronic strain
Vertebral body shape changes :
Biconcavity
Squaring
Wedging
Loss of normal wavy appearance
Chondrocalcinosis : knee (radiograph) (pseudogout)
Osteopenia, compression fractures: lumbar vertebrae (radiograph)
Compression fracture: lumbar spine (MRI)
Bone mineral density (BMD) measurements Measurement of BMD plays a central role in the investigation and management of osteoporosis. Dual energy X-ray absorptiometry (DXA or DEXA) is the current method of choice because of its sensitivity and low radiation dose.
Ultrasonography
Arthrography
Radionuclide bone scans
Magnetic resonance Computerised tomography (CT) and imaging (MRI)
Synovial Fluid (SF) Analysis
Fresh unrefrigerated sample to avoid:
Crystal dissolution
Post tapping crystallization
Diagnostic in:
Septic arthritis
Crystal associated arthritis (gout & pseudo gout)
Intra-articular hemorrhage
Helpful in other conditions
SF in joint diseases
Normal SF
Increase in cells
Few cells
Faint to marked turbidity
Clear
Pale yellow or turbid
Colorless or pale yellow occasionally whitish (white crystals or cholesterol)
Low viscosity, specially in inflammatory diseases
High viscosity
Microbes maybe detected in infective arthritis (gram stain , Z-N stain , culture)
Sterile
Early “RA”: First few months of symptoms, frequently a challenging diagnosis