بسم هللا الرحمن الرحيم
Cell Injury & Adaptations
Professor Dr. Wahda M.T.Al-Nueimy
Department of Pathology
College of Medicine
University of Mosul
2013

Cellular response to injury
•Cellular adaptations
•Atrophy, hypertrophy, hyperplasia, metaplasia.
•Acute cell injury
• Reversible injury ( cell degeneration ).
• Irreversible injury ( Cell death ).
• Necrosis
• Apoptosis
• Sub cellular alterations in sub lethal and chronic injury.
• Intracellular accumulations.
• Calcification.
• Cell aging.
What is the factors that determine the
fate of cells after injury?
1-Type of injury.
2-Severity of injury
( mild , moderate or severe).
3-Duration of exposure (
short or long duration).
4-Type and state of cells.
5-Adaptability of the cell.
6-cellular metabolism, blood supply and
nutritional status.
According to capacity of cell to division it divided into
High capacity (labile cell
) Nil capacity (permanent)cell
◦
Epidermis Neurons
◦
Gastrointestinal epithelium Cardiac muscle
◦
Respiratory epithelium Skeletal muscle
◦
Bone marrow
Low capacity (stable cell)
◦
Hepatocytes
◦
Pancreas
◦
Kidney
◦
Smooth muscle
◦
Bone
◦
cartilage
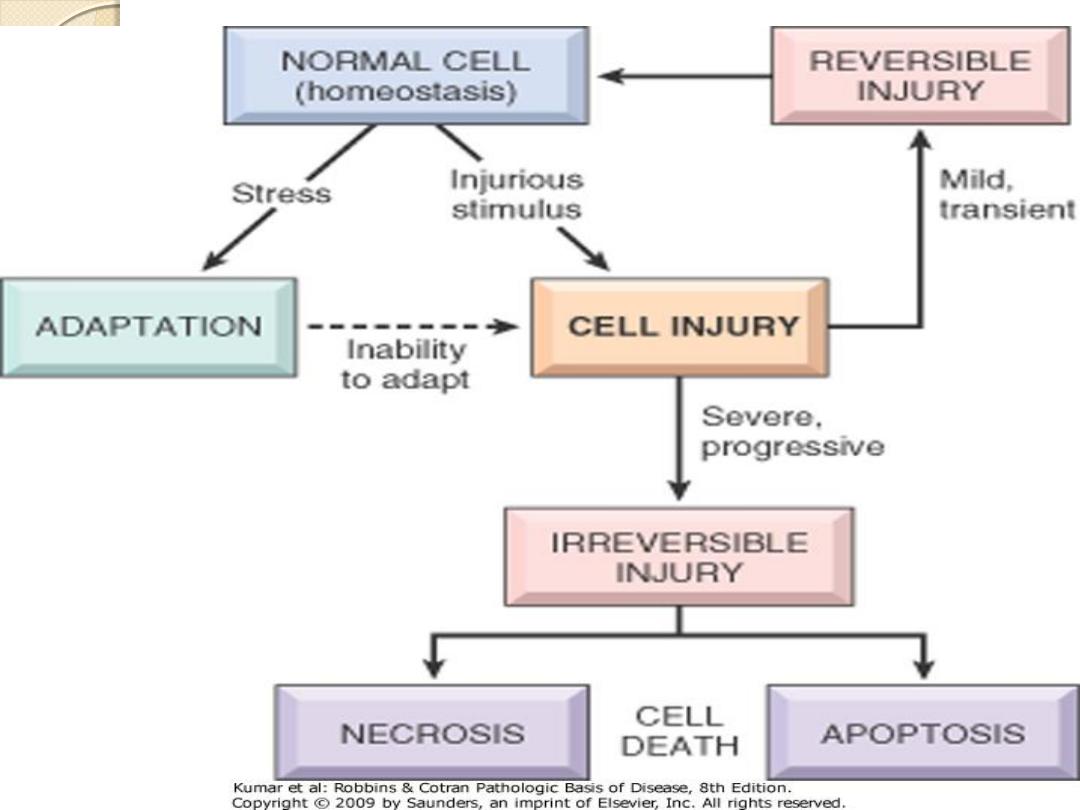

Acute Cell Injury ( short duration)
Reversible cell injury: indicates that the cellular
changes will
regress and disappear when the
injurious agent is removed; the cell will return
to normal both morphologically and
functionally.
Irreversible cell injury: occurs when the injury
persist or when it is severe from the start.
Here the
cell reaches the point of no return and
progression to cell death is inevitable
.

What is the causes of cell injury??
1-Hypoxia ( deficiency of oxygen)
◦
Ischemia ( decreased blood supply to tissue due to impeded arterial
flow or reduced venous drainage ) which is due to disease of blood
vessels.
◦
In adequate oxygenation of blood due to cardio-respiratory failure
and in CO poisoning ( CO forms a stable complex with hemoglobin
that prevents oxygen binding).
◦
If there is loss or reduction in the O2 carrying capacity ( anemia).
2-Physical injury
( extremes of temperature , radiation,
electrical shock, trauma, change in atmospheric
pressure )
3-Chemical agents, salt, glucose, oxygen, poisons,
pollutants, insecticides, asbestos, ethanol & drugs
.
4-Microbial agents i.e. mean infectious agents
(virus,
bacterial, fungal ,parasitic…..etc)

Chemical injury
There are
2
general classes of chemical injury
1- Direct interaction
with cellular component e.g.,
mercuric chloride cause membrane damage by binding
to sulfhydryl group of cell membrane.
2-Indirect interaction
by converted in the cell into
toxic metabolite
e.g., carbon tetrachloride change to
carbon trichloride free radical result in either
fatty
change or lipid peroxidation
.

Microbial injury
1-Direct induced injury
e.g. poliovirus cause direct
destruction of cell membrane of the host cell by
insertion of the virus into the cell membrane.
2-Indirect induced injury
e.g. hepatitis B virus
cause destruction of cell membrane of the cell by
stimulation of the immune system against the
viral protein
that exposed on the cell membrane.

5-Immunologic reactions e.g.
hypersensitivity
reaction which is mean exaggerated response of
the immune system , anaphylactic shock &
autoimmune diseases which is mean breakdown
of the normal tolerance mechanisms to self –
antigens.
6-Genetic abnormalities e.g.
Down’s syndrome
( trisomy 21) & sickle cell anemia
7-Nutritional imbalance
(vitamin deficiency,
protein deficiency, obesity , atherosclerosis,
cancer, alcoholism)
8-Aging.

Mechanism of cell injury (pathogenesis)
The susceptible targets in cell are:
1-Cell membrane destructed by
phospholipase
which secreted for example by certain bacteria.
Increased permeability of cell membranes
like
plasma membrane , lysosomal membrane leads to
necrosis.
2-ATP production lost by e.g., cyanide which inactivate
cytochrome oxidase in mitochondria causing
decrease
ATP production.
3-Protein synthesis .
4-defects in genetic apparatus.

5-
Accumulation of reactive oxygen species
which causes modification of cellular proteins,
lipids and nucleic acids.
6-
Accumulation of damaged DNA
and
misfolded proteins triggers apoptosis.

Cellular adaptations to stress
It is a state that lies intermediate between
normal, unstressed cell & the injured ,
over stressed cell.
It could be physiological or pathological
The adaptive responses include
1-Atrophy
2-Hypertrophy.
3-Hyperplasia.
4-Metaplasia.

Atrophy
It refers to the decrease in the size the organ as a result of
decrease in size of cells with loss of cell substances.
Cells exhibit
autophagy ( self eating)
with increase in
number of autophagic vacuoles & lipofuscin ( wear and tear
pigment).
causes: Pathological & physiological atrophy :
1-Decrease in the workload ( disuse).
2-Denervation: ( neuropathic) e.g. paralysis of limb due to
nerve injury or poliomyelitis.
3-Under nutrition as in starvation.
4-Loss of endocrine stimulation e.g. atrophy of the gonads
in hypopituitarism.
5-Aging it is called senile atrophy.
6-Diminish blood supply.


Hypertrophy
Refer
to increase in the size of organ as a
consequence of the increase of cell size
. It is due to
synthesis of more structural
component
as a result of
either increased functional demand or by specific hormonal
stimulation; occurs in tissue incapable of cell division.
It can be
physiological or pathological
e.g.,
◦
Uterus in pregnancy as a consequence of estrogen
stimulate smooth muscle fibers.
◦
skeletal m. in athletes, or manual workers in response to
increased demand, left ventricular hypertrophy
(pathological), Hepatocytes hypertrophy in barbiturate
drug therapy, Compensatory mechanism after
nephrectomy .
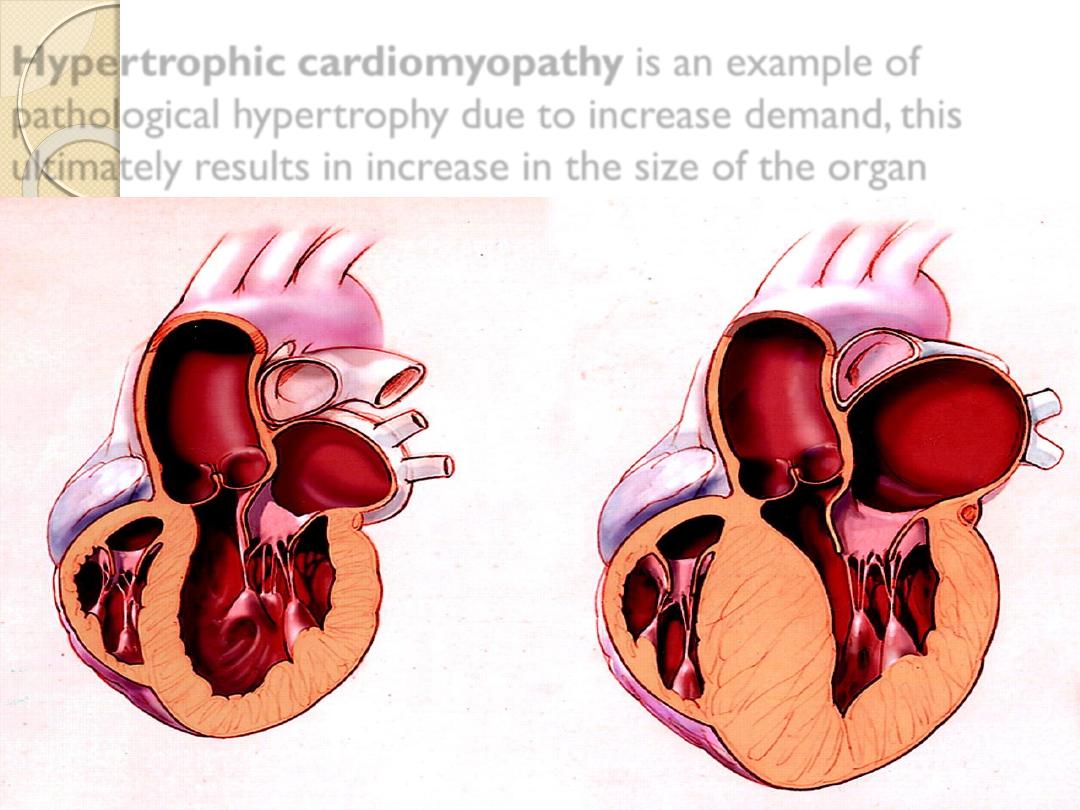
Hypertrophic cardiomyopathy
is an example of
pathological hypertrophy due to increase demand, this
ultimately results in increase in the size of the organ
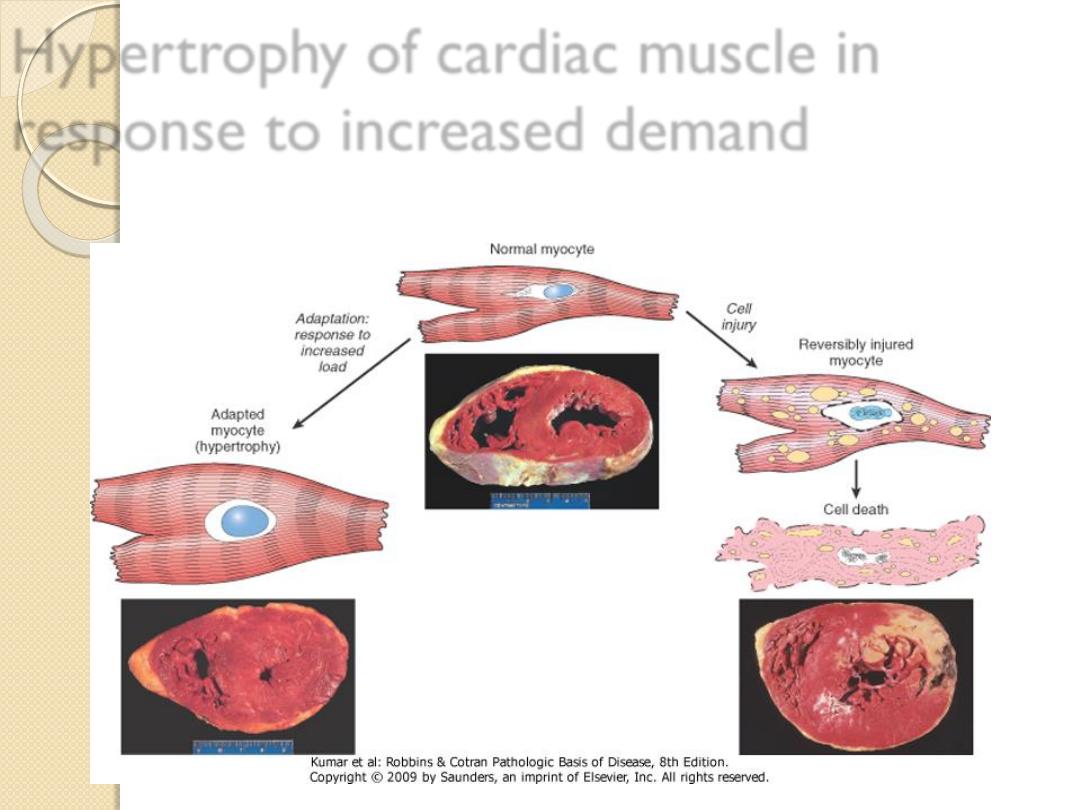
Hypertrophy of cardiac muscle in
response to increased demand

Hyperplasia:
It’s refer to the increase in the size of the organ as a result
of increase in the
number of cells, in response to
hormones and other growth factors.
Cells that undergo hyperplasia are those capable of cell division
(labile cells).
Hyperplasia is divided into:
Physiological: which is
◦
either
hormonal
(proliferation of the breast glandular epithelium of
female at puberty, or during pregnancy) , nodular prostatic
hyperplasia after age of 50.
◦
or
compensatory
(e.g. after partial hepatectomy).
Pathological:
Extensive hormonal stimulation
(e.g. endometrial
hyperplasia). Or
effect of growth factors
as in healing of wounds
forming keloid Or certain viral infections e.g. papillomaviruses cause
skin wart .
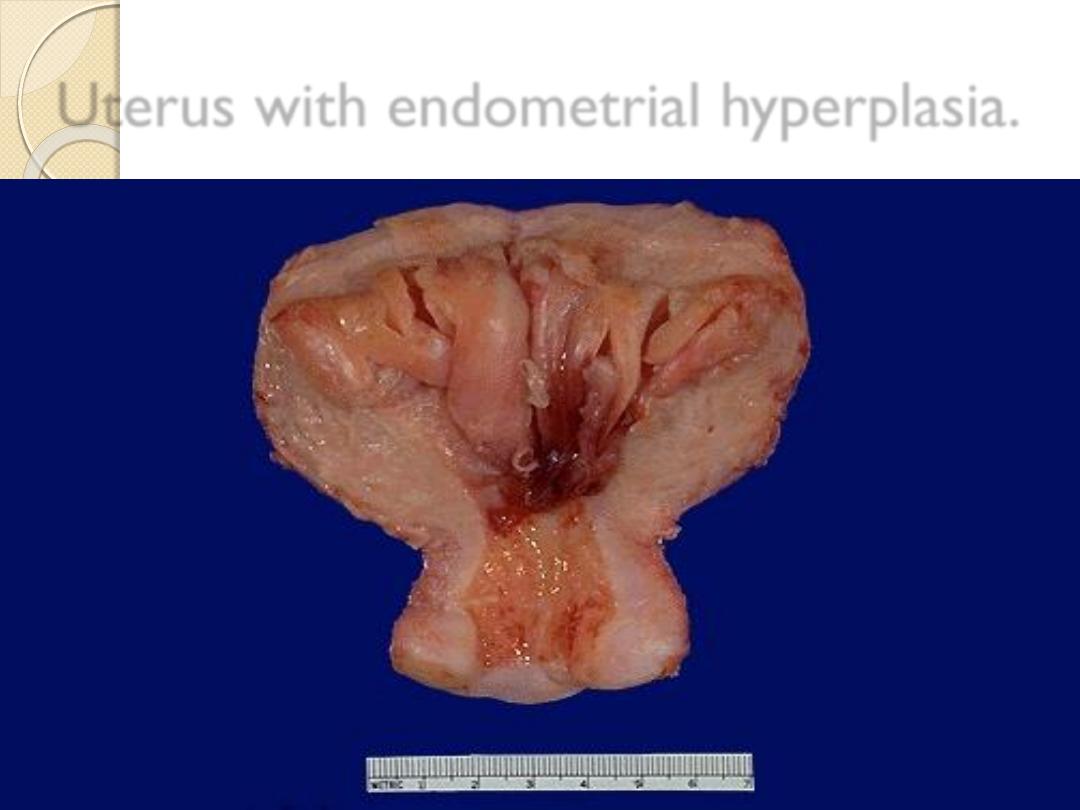
Uterus with endometrial hyperplasia.
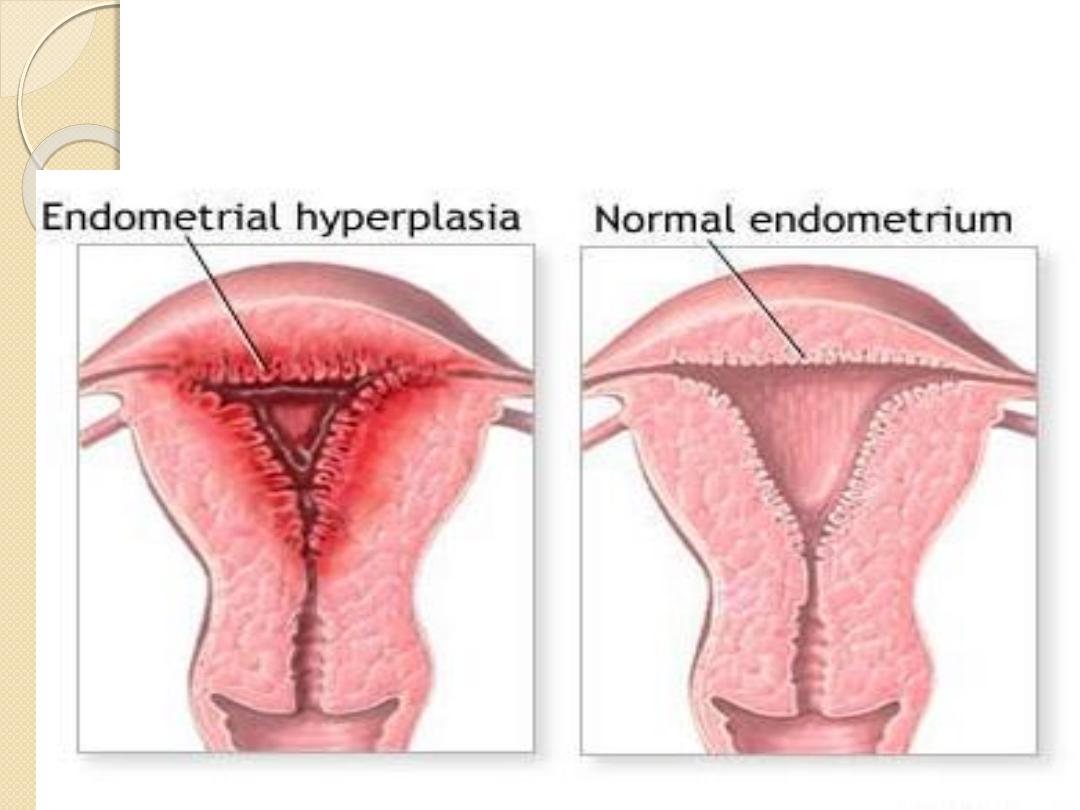
Endometrial hyperplasia is an example of hormone-
induced
hyperplasia
due to hyperestrogenism.
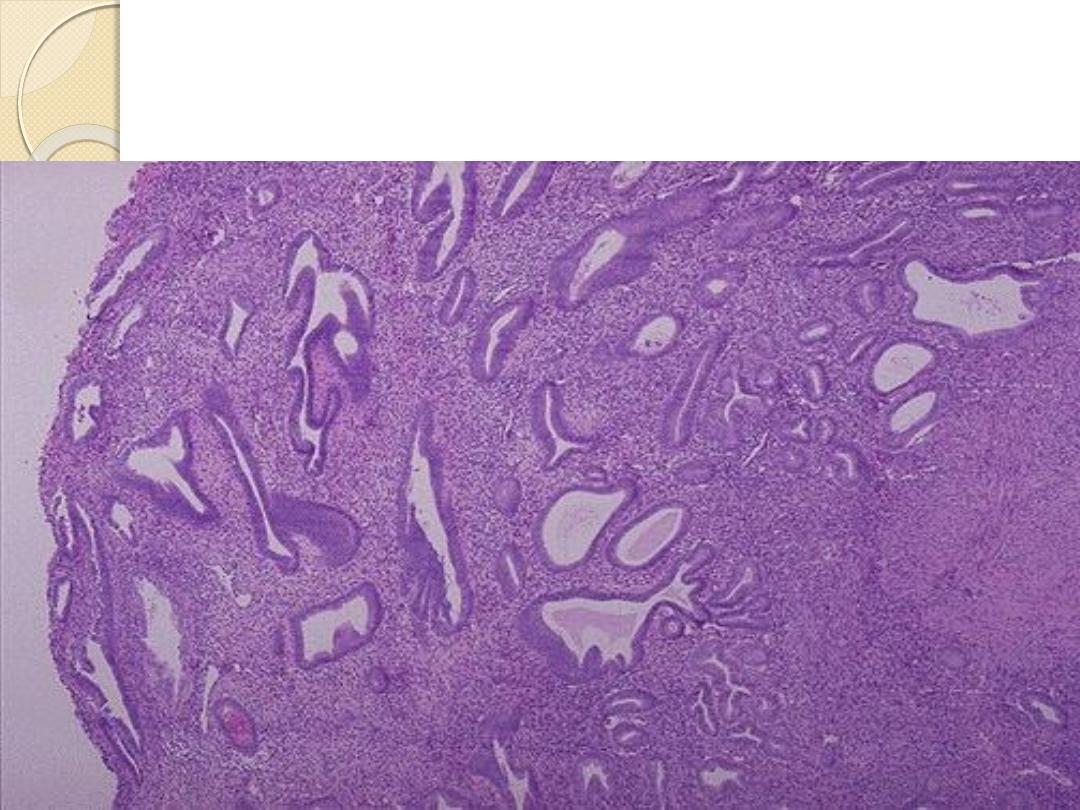
Endometrial hyperplasia-there is hyperplasia of the
both glandular & stromal elements.
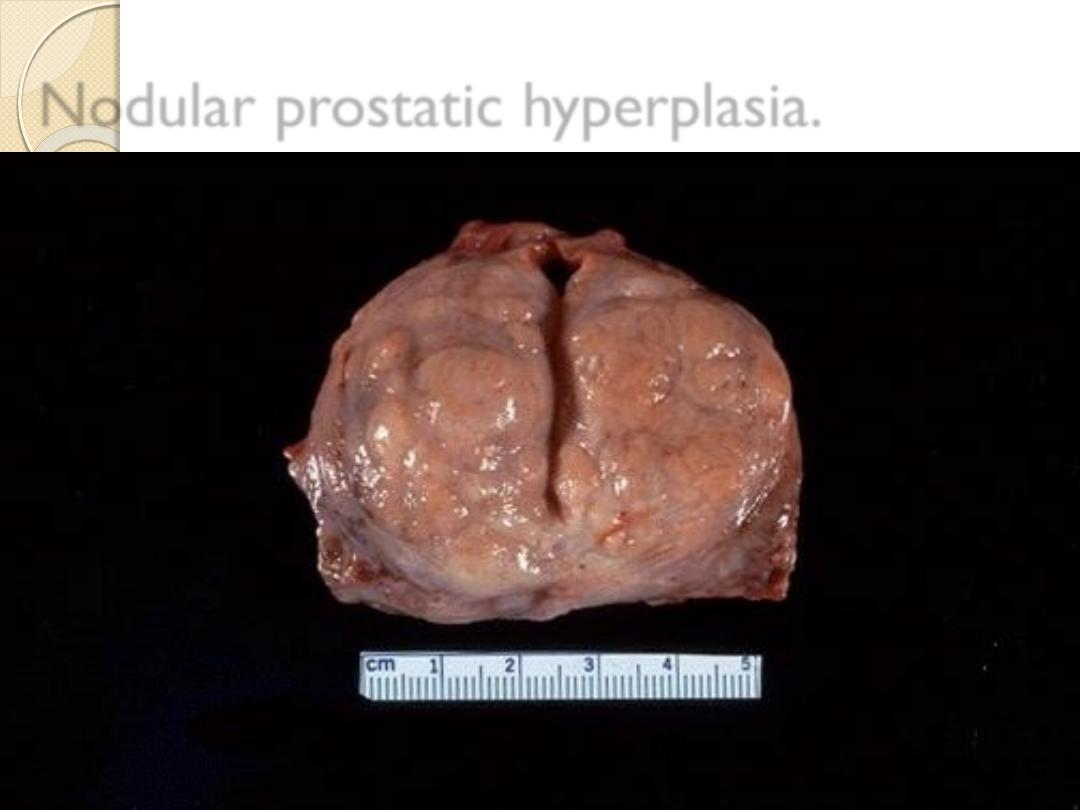
Nodular prostatic hyperplasia.

Hyperplasia is due to sensitivity to normal
regulatory control mechanisms that distinguish
benign pathologic hyperplasia from cancer, in which
the growth control mechanisms become
dysregulated or ineffective.
Nevertheless ,
pathologic hyperplasia constitutes
a fertile soil in which cancerous proliferation
may eventually a rise as in complex
endometrial hyperplasia.

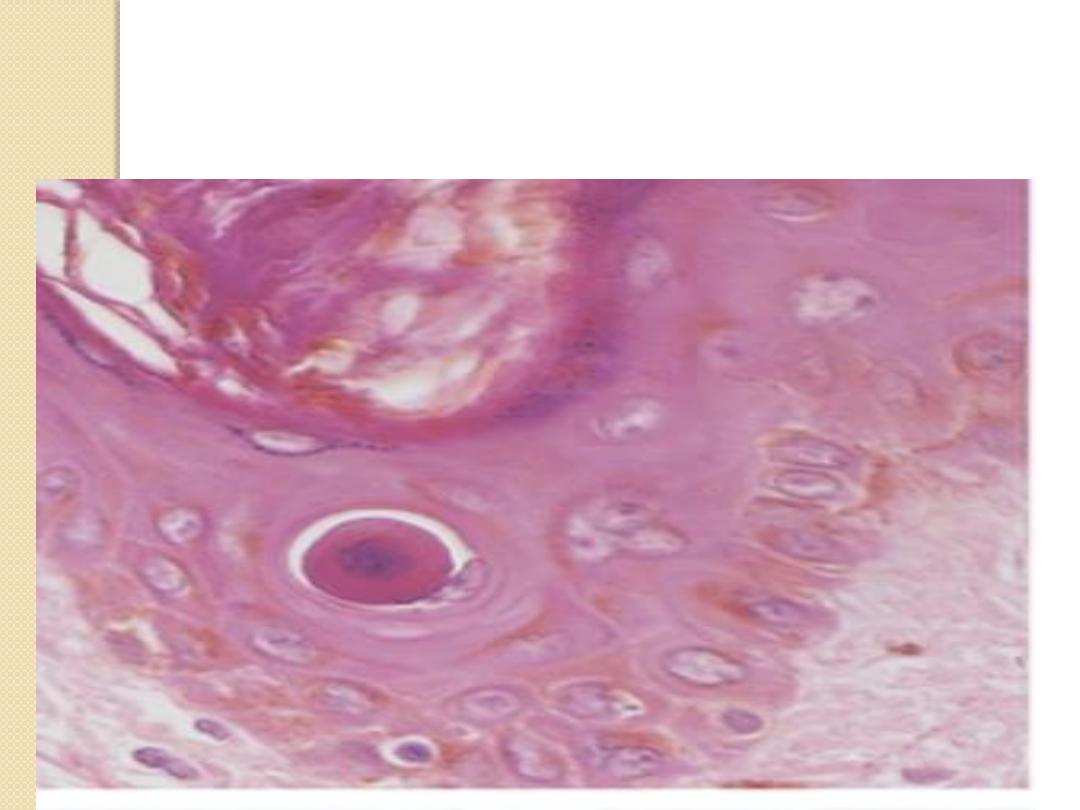
Metaplasia;
It’s refer to reversible , replacement of one mature cell type
by another mature cell type, which could be either epithelial
or mesenchymal , often a response to chronic irritation,
usually induced by altered differentiation pathway of tissue
stem cells; may result in reduced functions or increased
propensity for malignant transformation.
It is
an adaptive reversible process.
It may represents an adaptation of cells more sensitive to
stress by other that are more resistant to the adverse
environment. E.g.

Squamous metaplasia of the bronchial
respiratory epithelium due to habitual smoking.
Squamous metaplasia of the uterine cervix due
to continuous irritation by infection and sexual
intercourse.
Squamous metaplasia of urothelium of the
bladder due to bilharziasis or stone.
Columnar metaplasia of esophageal sq.
epithelium. as a result of prolonged reflux
esophagitis ( Barrett’s eosophagus).
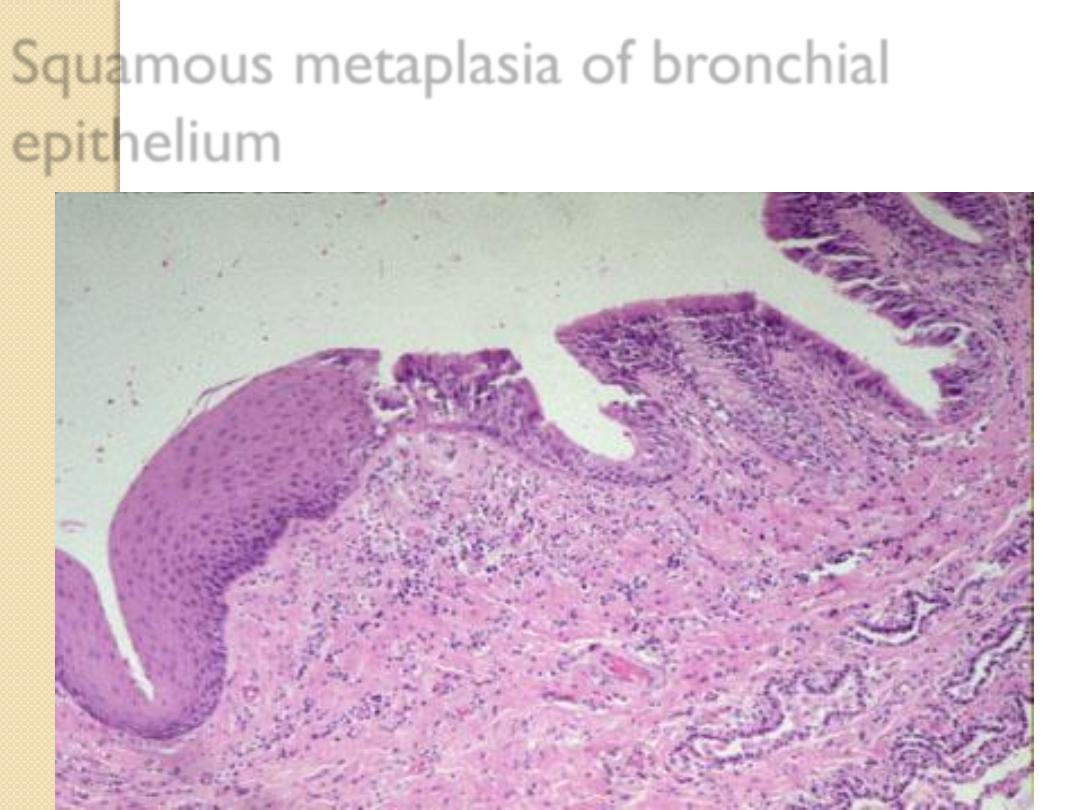
Squamous metaplasia of bronchial
epithelium
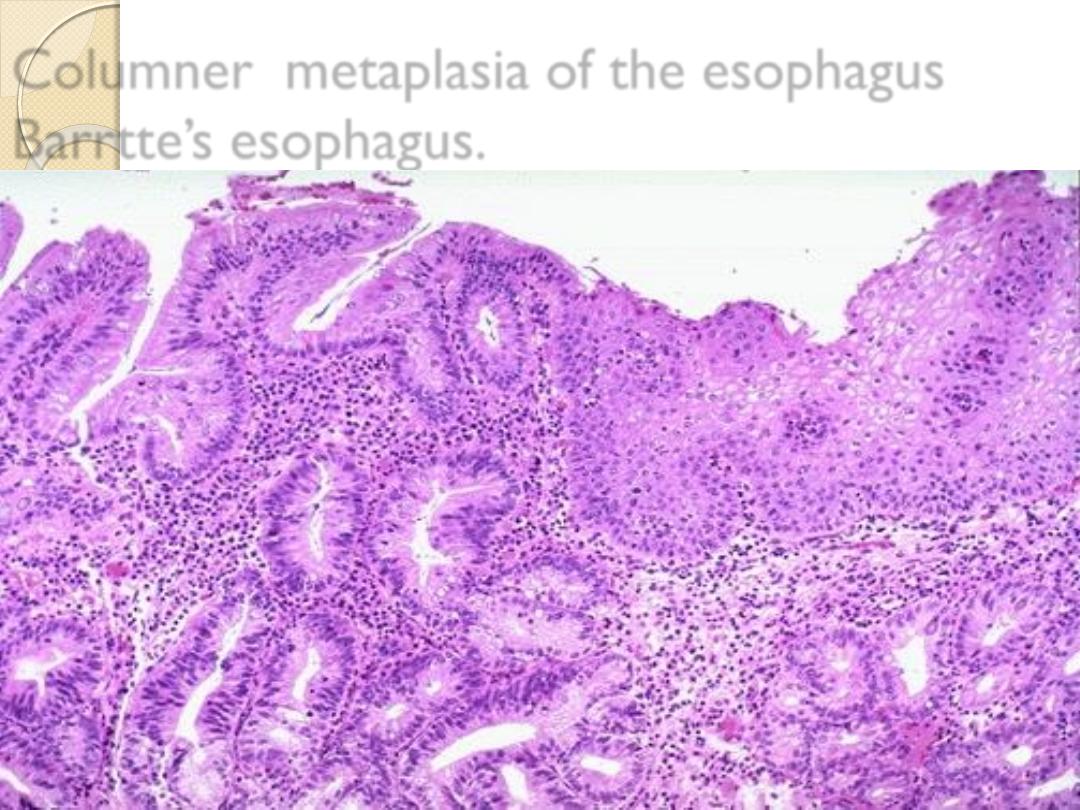
Columner metaplasia of the esophagus
Barrtte’s esophagus.

Metaplasia usually occurs as a result of
selective gene expression
depending on the
the site, need and environment.
Metaplasia in mesenchymal tissue is less common
and less important and
not precancerous
.
e.g. osteiod metaplasia may be seen in calcified
blood vessels, calcified hematoma, calcified colloid
within thyroid gland ----ect.

What are the mechanisms of irreversible cell
injury?
1-ATP depletion
reduces the activity of Na pump at the
cell membrane leading to gross changes in the intracellular
Na & K concentrations,t he net result is an influx of water
across the membranes causing the cell to
swell.
Continued ATP depletion interferes with protein
production.
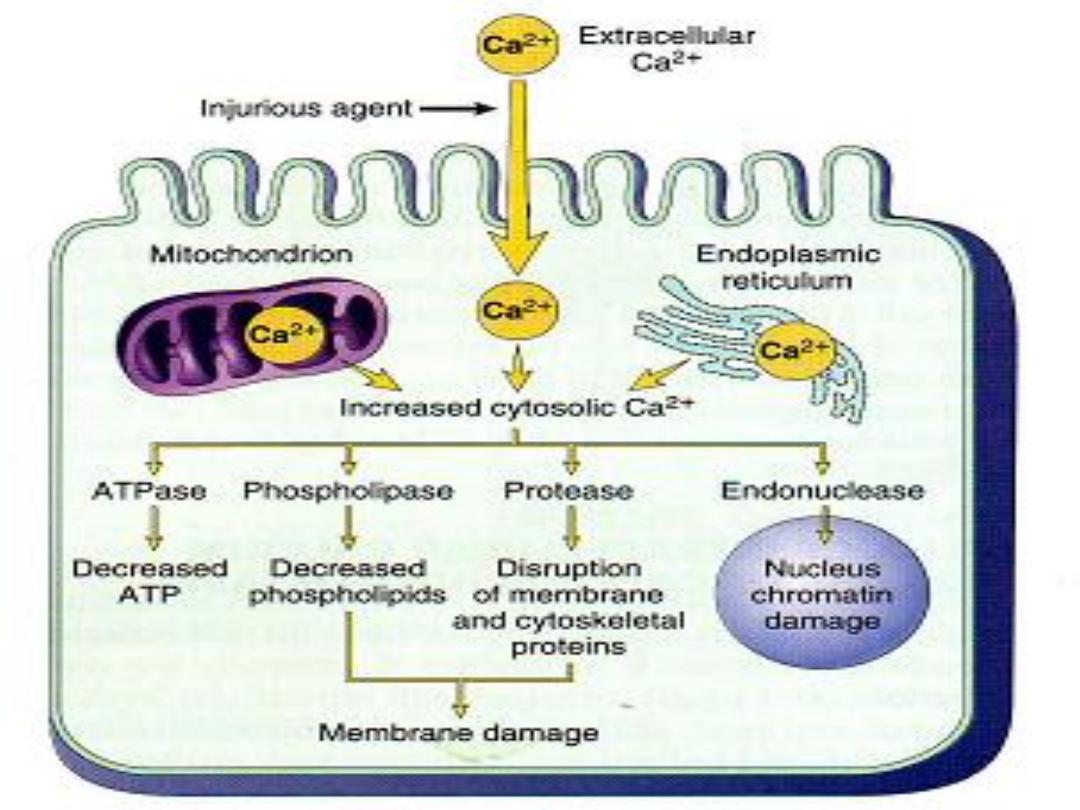
2-Cell membrane damage.
Cell membrane damage play the
Key factor
in the
pathogenesis of irreversible cell injury mediated by
excessive influx of calcium into the cell . Ca activate
cytosolic enzymes that could destroy cellular
components.

What is the mechanism of cell membrane
damage in irreversible cell injury??
Progressive loss of phospholipids.
Cytoskeletal alterations.
Lipid breakdown products.
- Free radical
induced injury by interact with lipids in
cell membrane resulting in lipid peroxidation , cellular
proteins, and DNA leading to breaks in its continuity .
The imbalance between free radical generation and
scavenging which occurs in injury is referred to as
oxidative stress.
Mitochondrial dysfunctioning.

Free radical induced injury
FR :are chemical species with a single unpaired electron in
the outer shell.
These are highly reactive & autocatalytic.
What is the source of free radicals?
1-endogenous (leukocytes, macrophages & endothelial
cells)
2-metabolites of drugs & chemicals.
3-Absorption of radiant energy.
Types of free radicals
◦
Superoxide, nitroxide , hydroxyl, hydrogen peroxide,
carbontrichloride CCL3.

Example of Free Radicals induced injury
Inflammation
as a part of defense mechanism.
Reperfusion injury
( this occurs following restoration of
blood flow in ischaemic tissues), cause release of FR from
leukocytes.
Aging process
decrease ability to handle with FR.
O2 toxicity
e.g. diffuse alveolar damage in lung.
Radiation
Chemical & drug injury
e.g., CCL3 cause severe injury in
the liver.

What is the targets of FR injury in the cells?
1- Membrane damage through the process of
lipid
peroxidation.
2- Cross linking proteins forming
disulfide bonds.
3- DNA: Single strand break in DNA & induction of
mutation
that interfere with cell growth leading to cell
death or eventual malignant transformation of cells.
4- Mitochondrail DNA is also affected.

Morphology of reversible cell injury:
By Light Microscope
◦
Cellular swelling result in large pale cytoplasm.
◦
Hydropic vaculation ( vacuolar degeneration).
◦
Fatty change.
◦
Clumping of chromatin.
By Electron Microscope
◦
Endoplasmic reticulum dilatation, Mitochondrial
dilatation , Cytoplasmic blebs & loss of microvilli ,
Detachment of ribosomes & dissociation of polysomes
into monosomes , Myelin figures and whole cell
swelling .

Morphological changes in irreversible cell injury
By E.M.:
◦
Breaks in the cell & organelles membranes.
◦
Amorphous large, bizarre form of calcification in
mitochondria .
◦
Rupture lysosomes
◦
Fragmentation of endoplasmic reticulum.
By L.M.:
◦
Nuclear changes including
Pyknosis
(nuclear shrinkage + increase basophilia of
the nucleus).
Karyorrhexis
(fragmentation with nuclear dust).
Karyolysis (
nuclear loss).

A nucleated cells
: have intensely eosinophilic
cytoplasm due to
◦
Loss of RNA .
◦
Glycogen depletion.
◦
Increased binding of eosin to denatured
intra-cytoplasmic protein.
Necrosis:
It is death of tissue or organ during
life
associated with
structural changes and with reaction from surrounding
living tissue
( inflammation) and initiation of a repair
process.
Mechanism of necrosis:
Denaturation of proteins
Enzymatic digestion by
◦
Autolysis by lysosomal enzyme of the cell itself.
◦
Heterolysis by surrounding inflammatory cells (Neutrophils &
Monocytes).
It is passive process, it is
a
ssociated with
inflammation, it r
andomly occurs .

Involve a group of cells.
Always pathologic.
Causes : chemical injury or infarction
( cell death due to cut of blood supply),
nutritional….etc
Types of necrosis:
Coagulative necrosis , most common .
Liquefactive necrosis.
Caseous necrosis.
Gangrenous necrosis (Gangrene).
Fat necrosis.
Fibrinoid necrosis.
Gummatous necrosis (Gumma).

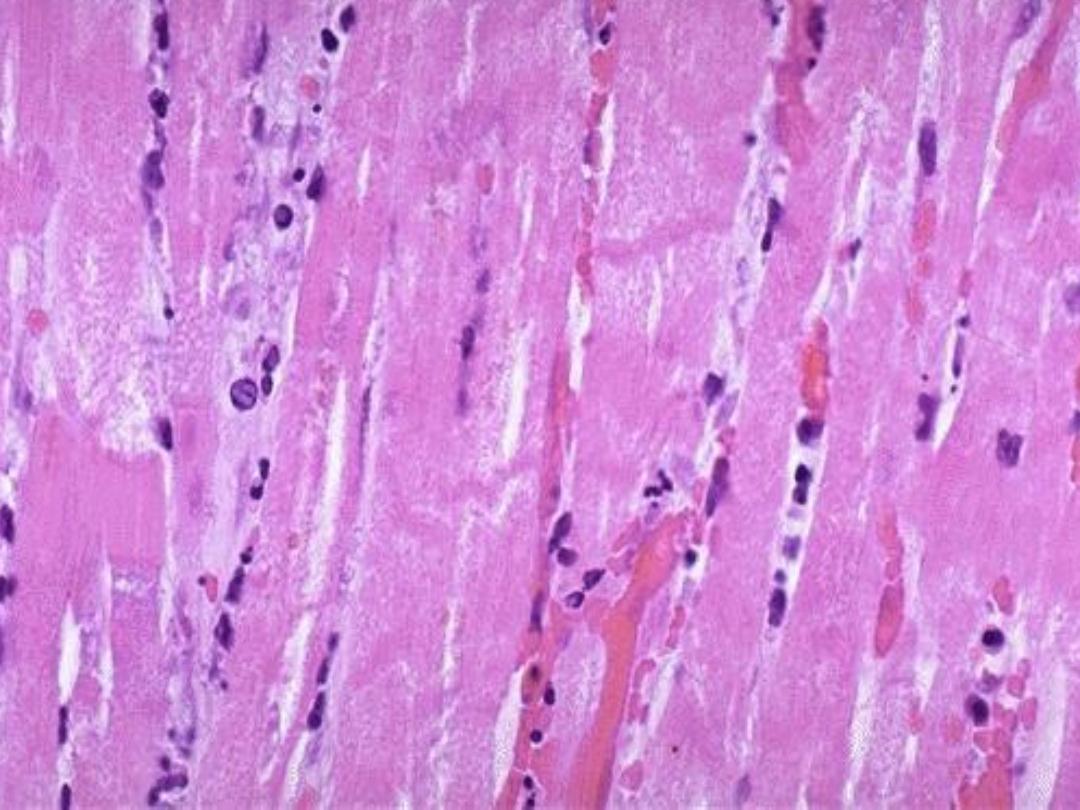
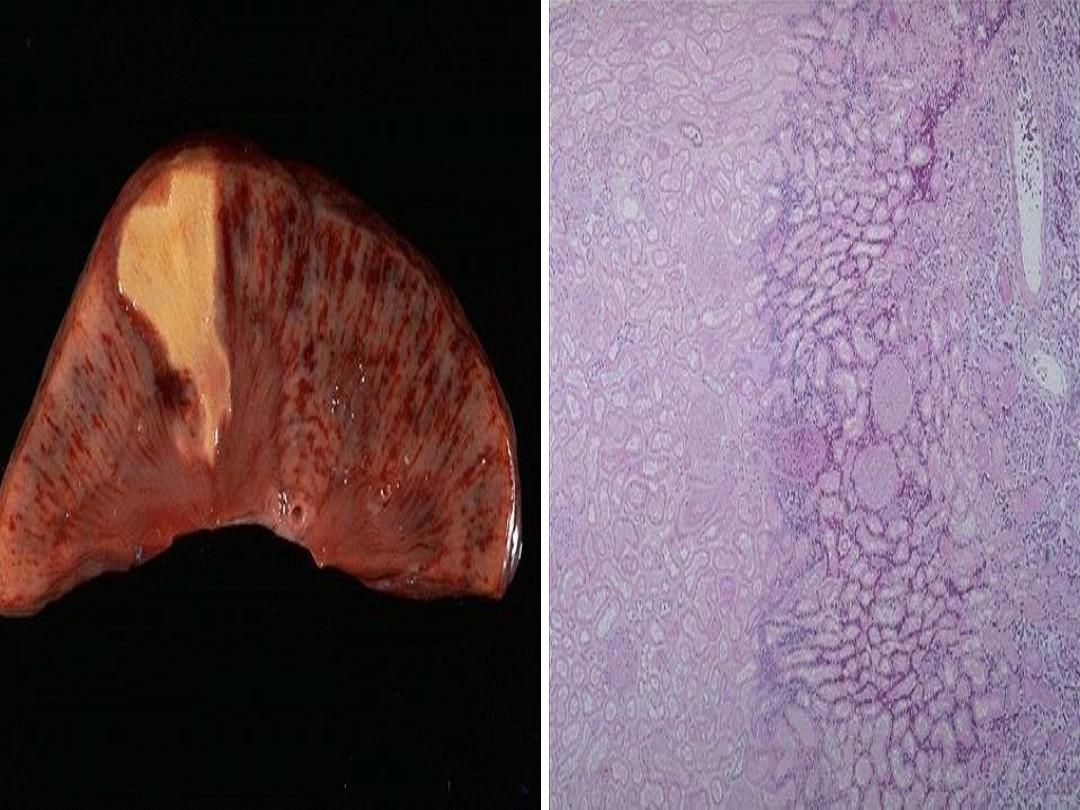
Coagulative necrosis
The commonest type of necrosis.
Infarcts (ischemic necrosis) in all
solid organs
except
the brain & spinal cord result in liquefactive necrosis.
Grossly:
◦
Whitish-gray or red-hemorrhagic firm wedge shape area of
infarction.
Histology:
◦
Preservation of the tissue architecture & cellular outline for
sometime with loss of internal details including nuclei.
◦
Result from denaturation of all proteins including enzyme as a
result of ischemia & acidosis
Fate:
after several days
fragmentation &
phagocytosis then healing .
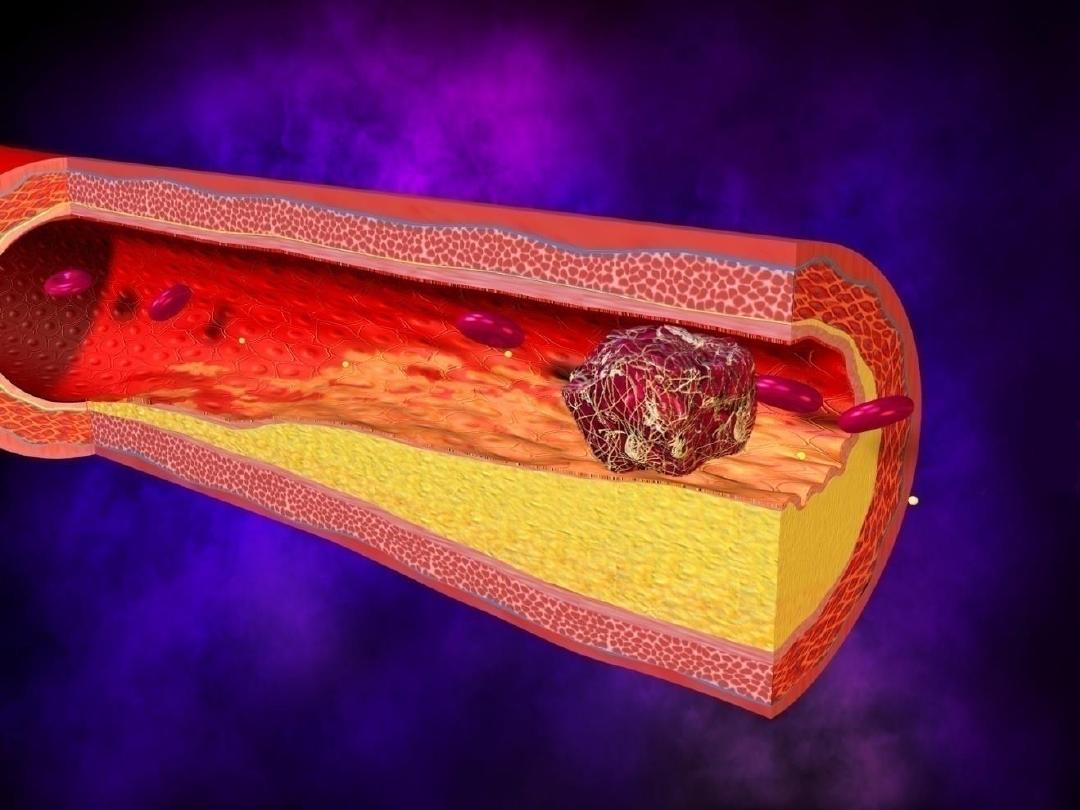
infarction
It is an ischemic necrosis caused by occlusion of
either the arterial supply or the venous
drainage.
Necrosis is of coagulative type as in myocardial
infarction (except brain: liquifactive CVA ).
The necrotic zone is an infarct area.
classification
Infarcts are classified on the basis of their color
into:
1-Red(haemorrhagic).
2-White(anemic).
and on the presence or absence of infection into:
1-Septic.
Is usually restricted to infarcts caused by
septic embolus.
The bacteria in the embolus invade
the dead tissue and causes suppuration, initially at the
margin, and then the infarct is converted to an
abscess.
2-Sterile.
Red infarct
(haemorrhagic)
Venous occlusion
(testis , ovary).
Loose tissue that allow the blood to collect in
the infarcted zone
(lungs).
Tissues with
dual
circulation e.g. (lungs,
small intestine).
Previously congested tissues (from sluggish
venous flow).
Reperfusion of previously ischemic tissue
(following angioplasty of an arterial
obstruction).

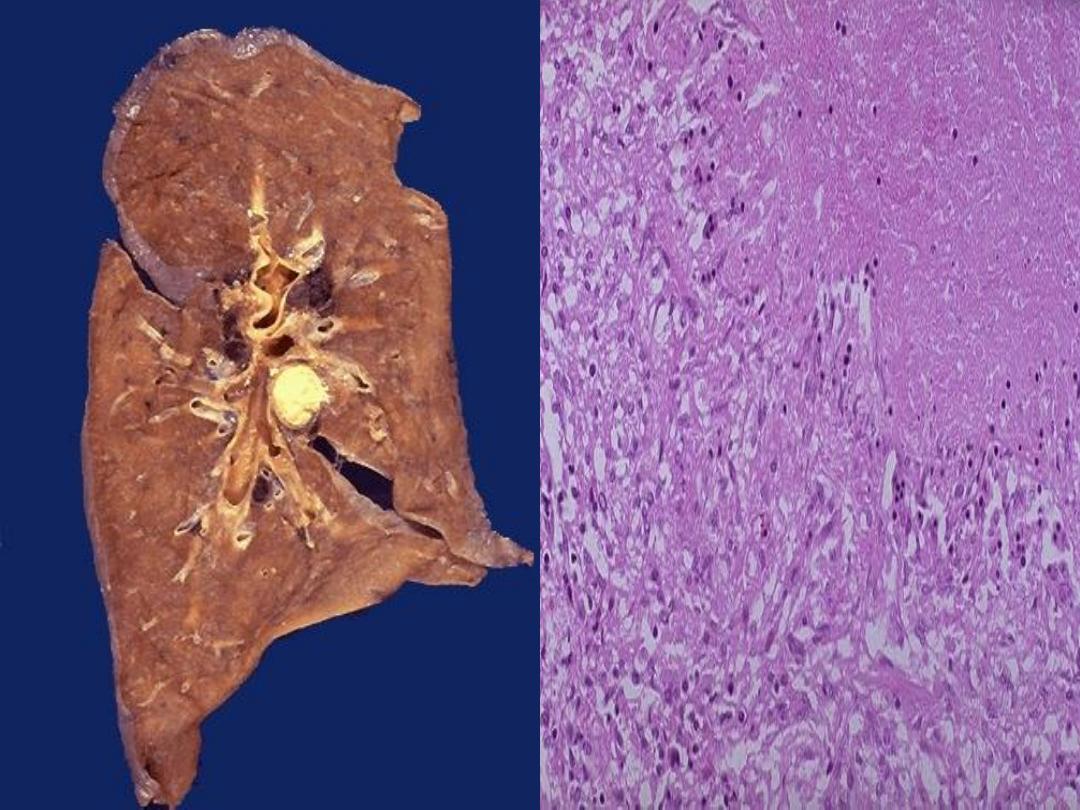
LUNG INFARCT
Grossly,
red infarcts are
sharply circumscribed,
firm and dark red to
purple.
Over a period of
several days, acute
inflammatory cells infiltrate the
necrotic area from the viable
border. The cellular debris is
phagocytosed and digested by
polymorphonuclear leukocytes
and later by macrophages.
Granulation tissue eventually
forms, to be replaced ultimately
by a scar.

Pulmonary infarction produced by a medium-sized thromboembolus
to the lung.
This infarction forms a wedge- shaped
area
& has begun to organize at the margins.
White infarct (anemic)
Occur in the arterial occlusion in solid organs with end-
arterial circulation
(spleen, kidneys & heart).
Most infarcts tend to be wedge-shaped,with the
occluded vessel at the apex
and the periphery of the
organ forming the base.
On gross examination, 1 or 2 days after the initial
hyperemia, the infarct becomes soft, sharply delineated, and
light yellow
due to denaturated cellular proteins which
resist digestion by proteiolytic enzymes
.
The border tends to be dark red, reflecting hemorrhage
into surrounding viable tissue.
Microscopically, a pale infarct exhibits uniform coagulative
necrosis.
Splenic infarct
It’s conical and subcapsular , at first the infarcted
tissue is dark red due to congestion, but after a few
days it changes to pale yellow, before being slowly
organized to leave a depressed scar.
spleen has
single circulation
and the vasculature
is subdivided into segmental and subsegmental
arteries which supply wedge-shaped sectors that is
why the area appears
wedge in shape.

The effects of vascular occlusion can range from
NO or
minimal effect to causing the
death
of a tissue or person.
The major determinants of the eventual outcome are:
1-
Nature of the vascular supply
The availability of
an alternative blood supply
is the most important determinant of whether
vessel occlusion will cause damage. The lungs, liver,
hand and forearm, have
dual
blood supply so
they are relatively resistant to infarction. In contrast,
renal and splenic circulations are end-arterial
and vascular obstruction generally causes tissue
death.

2-
Rate of occlusion development
.
Slowly developing occlusions are less likely to cause
infarction, because they provide time to develop
alternate perfusion pathways.
3-
Vulnerability to hypoxia
. Neurons undergo
irreversible damage when deprived of their blood
supply for only 3 to 4 minutes. Myocardial cells are also
quite sensitive and die after only 20 to 30 minutes of
ischemia. In contrast, fibroblasts within myocardium
remain viable even after many hours of ischemia.
4-
Oxygen content of blood
. A partial obstruction
of a small vessel that could be without effect in an
otherwise normal individual might cause infarction in
an anemic or cyanotic patient.

Liquefactive necrosis
Early softening & liquefaction of the necrotic
tissue.
Proteolytsis over protein denaturation.
Seen in
◦
Ischemic necrosis
of CNS.
◦
Abscess
formation in pyogenic or fungal infection.
Gross
◦
Soft liquid like
Histology
◦
Loss of original tissue .

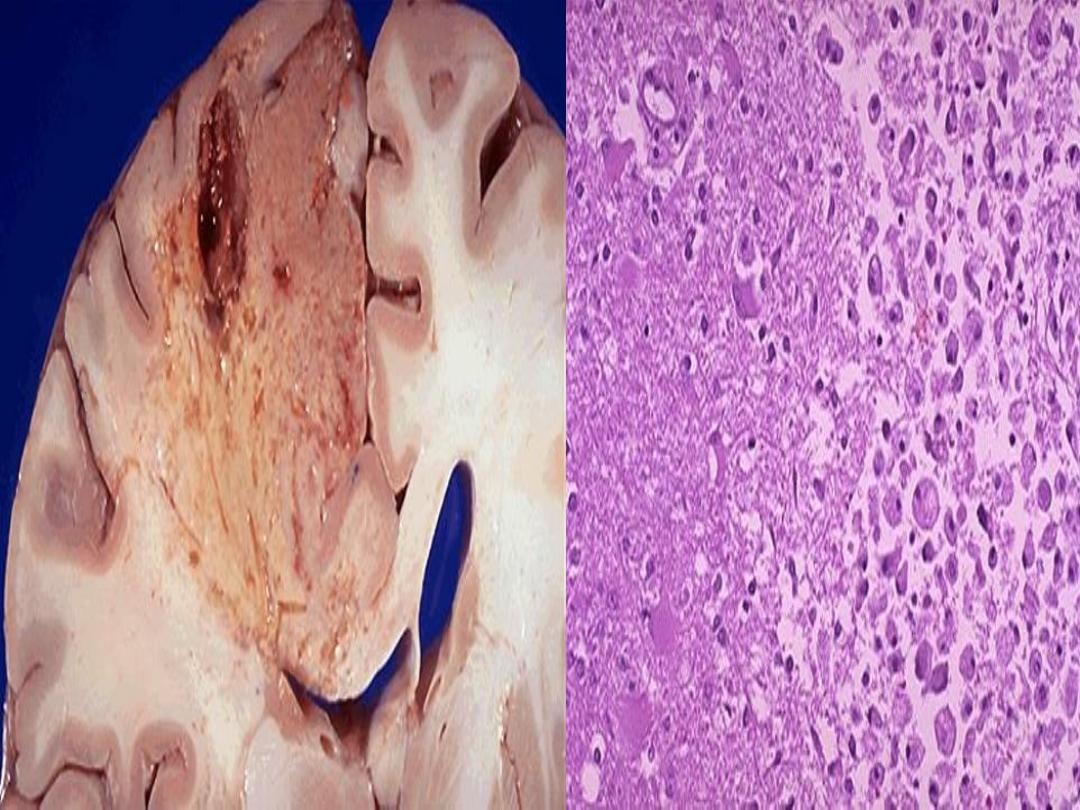
Liquefactive necrosis- Brain infarction

Caseous necrosis
it is a combination of coagulative and liquefactive
necrosis.
Being soft & yellow white appears as
cheese-like gross
appearance
Histology:
◦
Tissue architecture is completely loss.
◦
Appears as a brightly eosinophilic & amorphous
structureless material with nuclear dust.
Characteristic of
Tuberculosis(TB)
:
Coagulative necrosis modified by
capsule lipo-
polysaccharide of TB bacilli.
It could be seen in other lesions so it is not pathognomonic
of TB e.g. necrosis of tumor & inspissated pus.
Fat necrosis
Necrosis of adipose tissue,
characterized by the formation
of small quantities of calcium
soaps when fat is hydrolyzed
into glycerol and fatty acids. Also
called
steatonecrosis
.
A term for necrosis in fat, caused
either by release of
pancreatic
enzymes
from pancreas or gut
(enzyme fat necrosis) or by
trauma to fat
, either by a
physical blow or by surgery
(traumatic fat necrosis).

Fat necrosis
1-Enzymatic fat necrosis:
◦
In acute hemorrhagic pancreatitis cause activated lipase
leading to adipose tissue destruction causing releasing of
triglycerides & fatty acid.
◦
Deposition of calcium ending in calcium soap, grossly
visible chalky white areas.
2-Traumatic fat necrosis:
◦
Trauma to the
breast
causing rupture of fat cells
resulting in foreign body granulomatous reaction
◦
Ending in fibrosis & calcification causing stony hard
lump which is easily misdiagnosed by carcinoma of
breast clinically ,
definite diagnosis by biopsy.
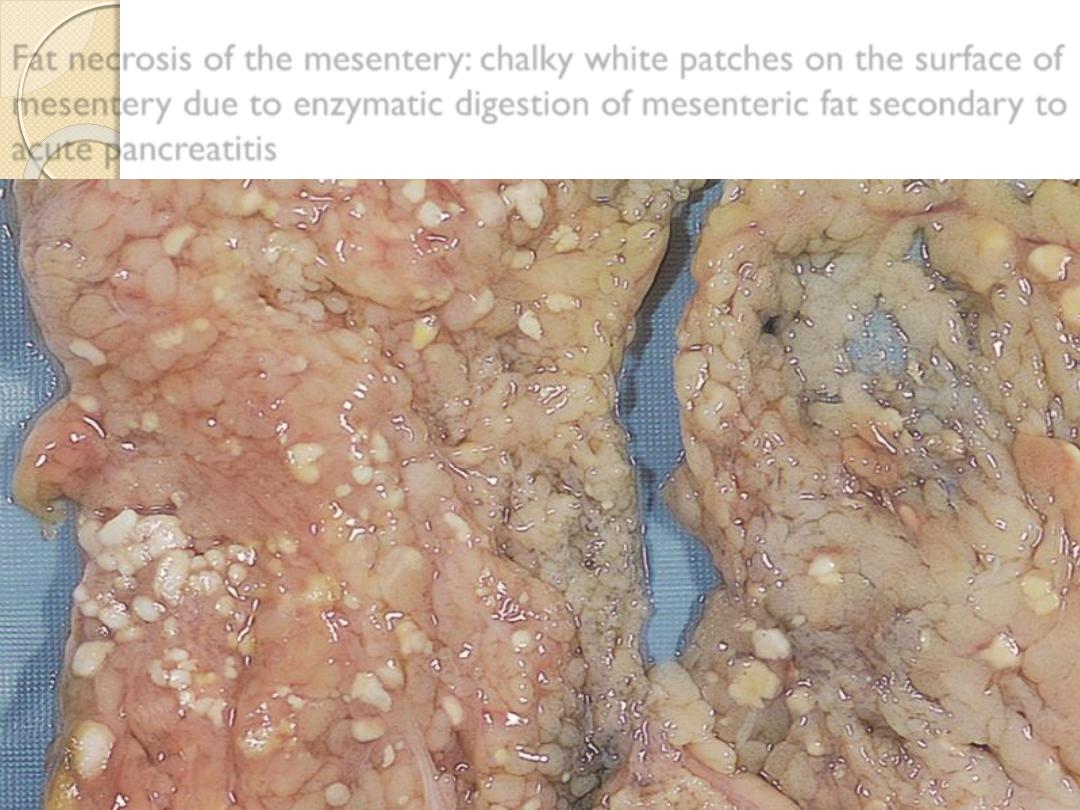
Fat necrosis of the mesentery: chalky white patches on the surface of
mesentery due to enzymatic digestion of mesenteric fat secondary to
acute pancreatitis
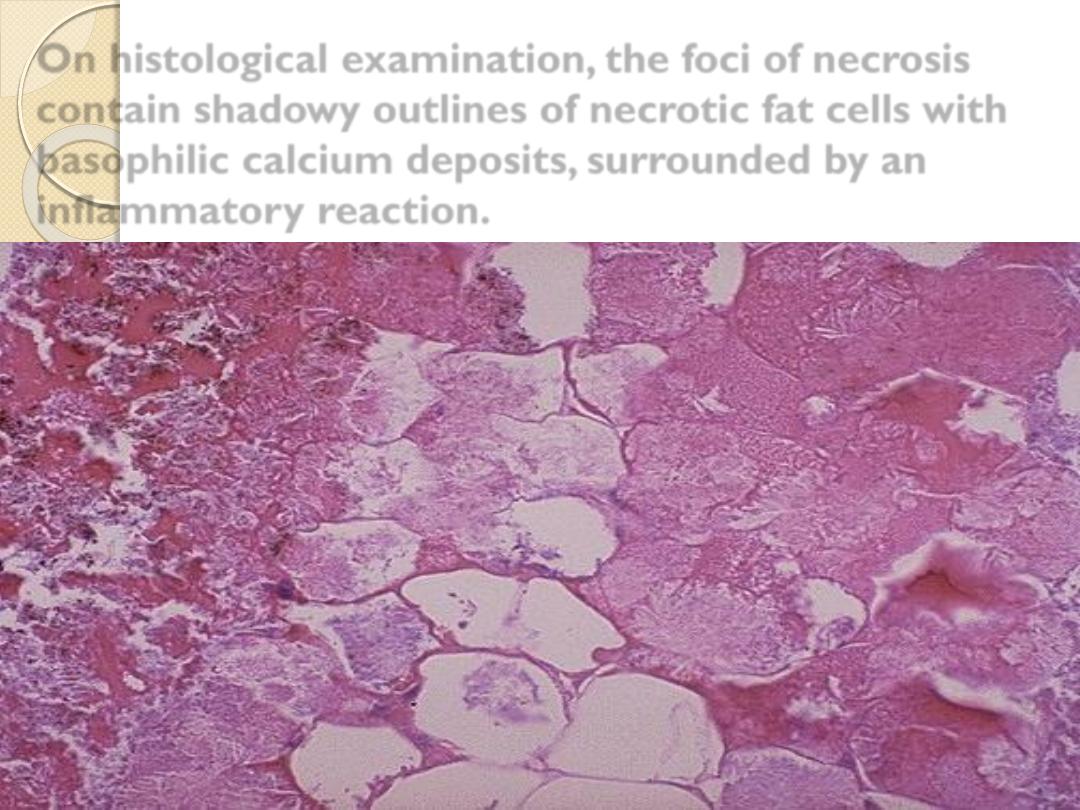
On histological examination, the foci of necrosis
contain shadowy outlines of necrotic fat cells with
basophilic calcium deposits, surrounded by an
inflammatory reaction.
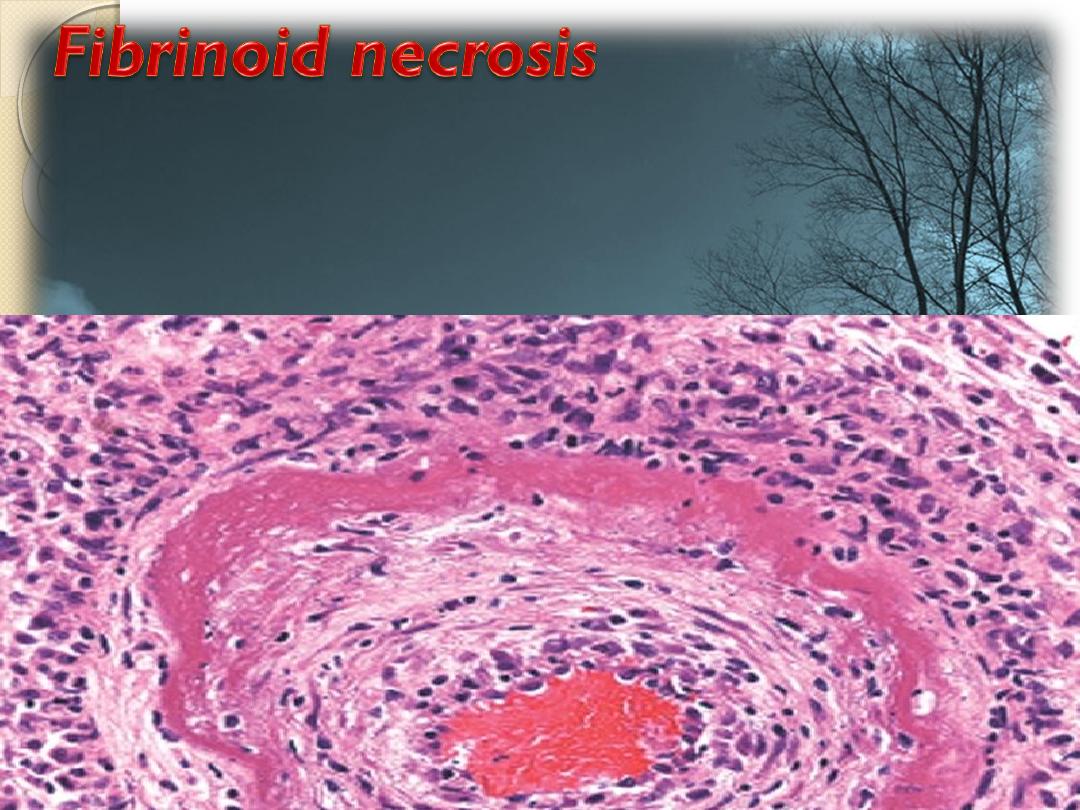
It’s caused by immune-mediated vascular damage.
It is marked by deposition of fibrin-like proteinaceous
material in arterial walls e.g. polyarteritis nodosa ,
which appears eosinophilic on light microscopy.
Artery,
fibrinoid necrosis

Fibrinoid necrosis
By Hematoxyline & eosin ( H&E ) it appears as
intense eosinophilic staining of involved
(necrotic) tissue, like fibrin.
It’s characterized by platelet activation, fibrin deposition
and usually cell death of the vascular smooth muscle.
Example:
Fibrinoid necrosis of blood vessels in
malignant
hypertension & vasculitis.
Fibrinoid necrosis of collagen tissue in connective tissue
disease as in
rheumatoid arthritis ( RA )
.
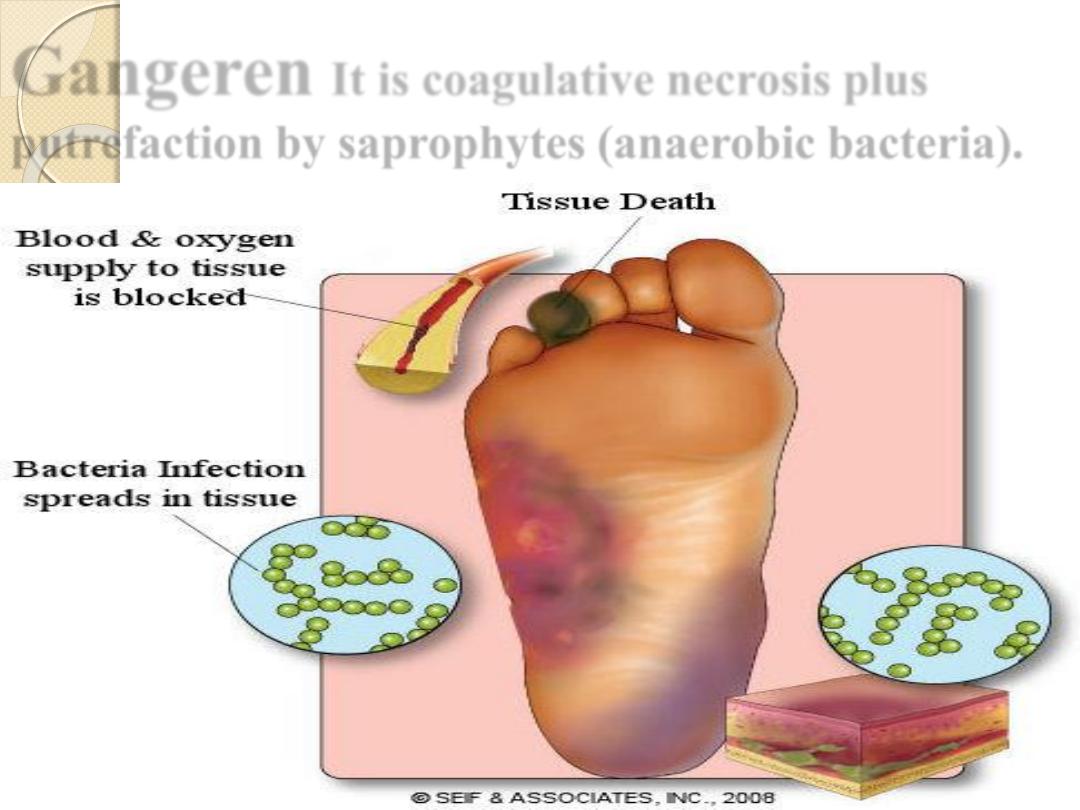
Gangeren
It is coagulative necrosis plus
putrefaction by saprophytes (anaerobic bacteria).

Gangrene
It can be classified into two types according to the
cause
of the tissue necrosis:
Primary gangrene:
It is brought by infection with
pathogenic bacteria which both kill the tissue by
secreting exotoxins & then invade & digest the dead
tissue.
Secondary gangrene
Secondary gangrene
This type of gangrene is characterized by necrosis
due to some other causes , usually loss of blood
supply from vascular obstruction or tissue laceration
& saprophytic bacteria then digest the dead tissue ,
there are two types :
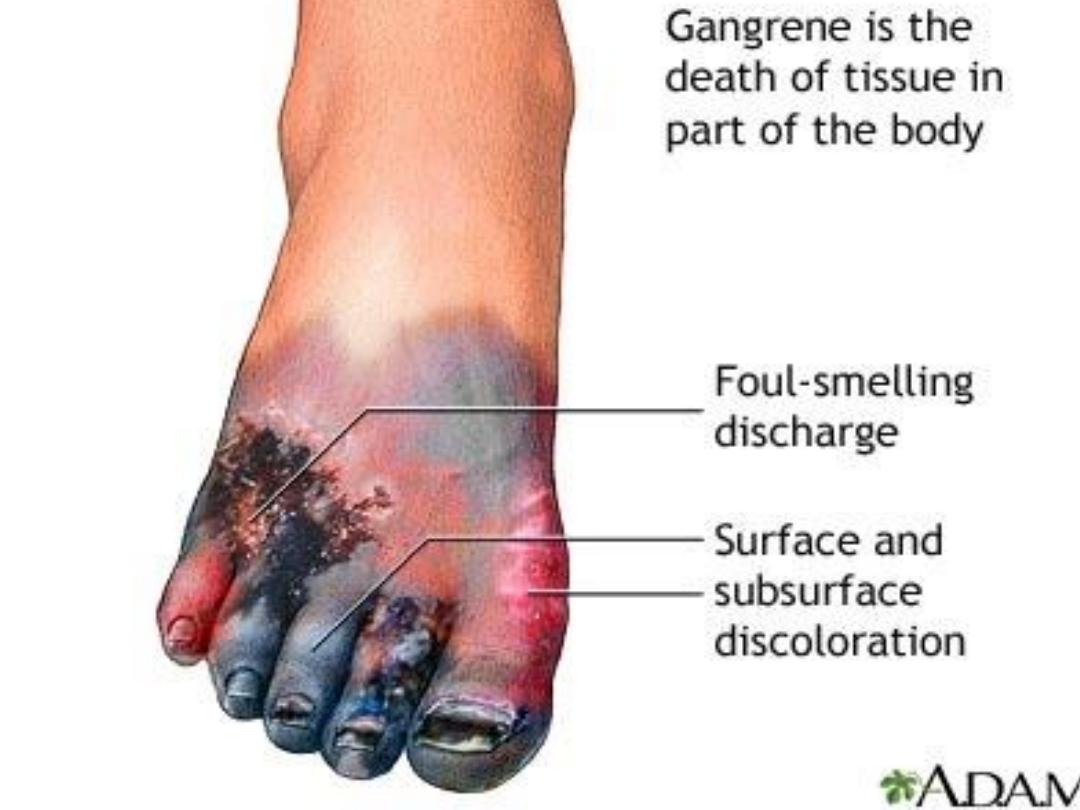
Dry gangrene
Wet gangrene

It is a form of a necrosis of the tissue with
superadded putrefaction.
Dry gangrene -Ischemia
Wet gangrene –D.M
Dry gangrene
There is drying & mummification of dead tissue.
It is seen in distal parts of the lower limbs
associated with peripheral vascular diseases
(atherosclerosis, vasculitis).
Due to gradual cut of blood supply.
The line of demarcation between dead and living tissue
is
clear.
The lesion remains
localized
.
Wet gangrene
The infected tissue are edematous due to large
amount of subcutaneous fluid.
The demarcation between dead and living is
extend proximally
beyond the site of infective.
Wet gangrene is seen in the bowel due to
mesenteric vascular occlusion and in diabetic
limb.

Gummatous necrosis
Derived its name from gumma , which is a
necrotic lesion seen in the
tertiary syphilis .
It is modified type of coagulative necrosis.

Fate of necrotic tissue
Body treats necrotic tissue as
a foreign materials.
It stimulates
an inflammatory
reaction that eventually
removes the necrotic tissue & prepare the scene for the
process of
repair
by:
◦
Regeneration ( return to normal state).
◦
Organization ( granulation tissue formation and
fibrosis).
These required proliferation, migration, differentiation of
cells & production of extracellular matrix.
Cyst formation like abscess.
Dystrophic calcification.
Effects of necrosis depend on the
1- Organ affected.
2- The extend of necrosis.
3- The duration of necrosis.
Death of cells from certain organs associated with
release of certain enzymes which could be used as
a sign or indication of necrosis
e.g.
SGPT
in death of liver cells.
SGOT & Troponin
in death of heart muscles
( Myocardial infarction).

Apoptosis ( falling off)
Death of single cell as a result of the activation of a
genetically
programmed (suicide) pathway
through
which the cell removed with minimal damage to the
tissue containing them.
It is very important part of the turn –over mechanism.
There are 3 major phases of apoptosis;
1- initiation or induction 2- execution 3- phagocytosis.

How the process of apoptosis is initiated?
Different types of stimuli causing activation of caspases
enzymes, which play the key role in the apoptosis, this activate
cytoplasmic endonuclease, proteases & transglutaminase.
Endonuclease
cleavage the DNA into fragments of double
stranded DNA.
Protease
degrade cytoskeleton & nuclear proteins .
Transglutaminase
cause cross linking of cytoplasmic
proteins causing shrinkage of the cells.
After that the cytotoxic T – lymphocytes release compounds
such as granzyme B which lead to the executioner phase
without the involvement of a transmembrane death receptor
complex or mitochondrial changes.

Genetic basis of apoptosis:
bax, bcl-x & bad genes are
apoptotic gene.
P53 stimulate apoptosis by stimulating
synthesis of bax gene.
bcl-2 is
anti-apoptotic gene
seen in
B-cell follicular lymphoma .

Examples where apoptosis occurs include:
a-Physiological apoptosis
mean elimination
unwanted cells
1-During embryogenesis; i.e. it is responsible for shaping
various organs and structures .
2- Hormone- dependent involution. e.g. of endometrium
during the menstrual cycle & lactating breast after
weaning.
3-Proliferating cell populations: e.g. intestinal epithelium,
skin & blood cells.

b-Pathological
apoptosis it occurs after some forms of cell
injury, especially DNA damage.
1-Atrophy of the prostate
after castration
.
2-Virally infected cells attacked by
cytotoxic T -
lymphocytes, as in
acute viral hepatitis (Councilman body).
3- Neoplasia.
4-Radiation.
5-Cytotoxic drugs .
6-Some mature B & T lymphocytes cannot distinguish self from non
self antigens, if that remain, will lead to destroy healthy body cells
(autoimmune disease).
7-Dermatosis (Civette bodies).
In apoptosis; nuclear chromatin condensation; formation of apoptotic
bodies ( fragments of nuclei and cytoplasm)
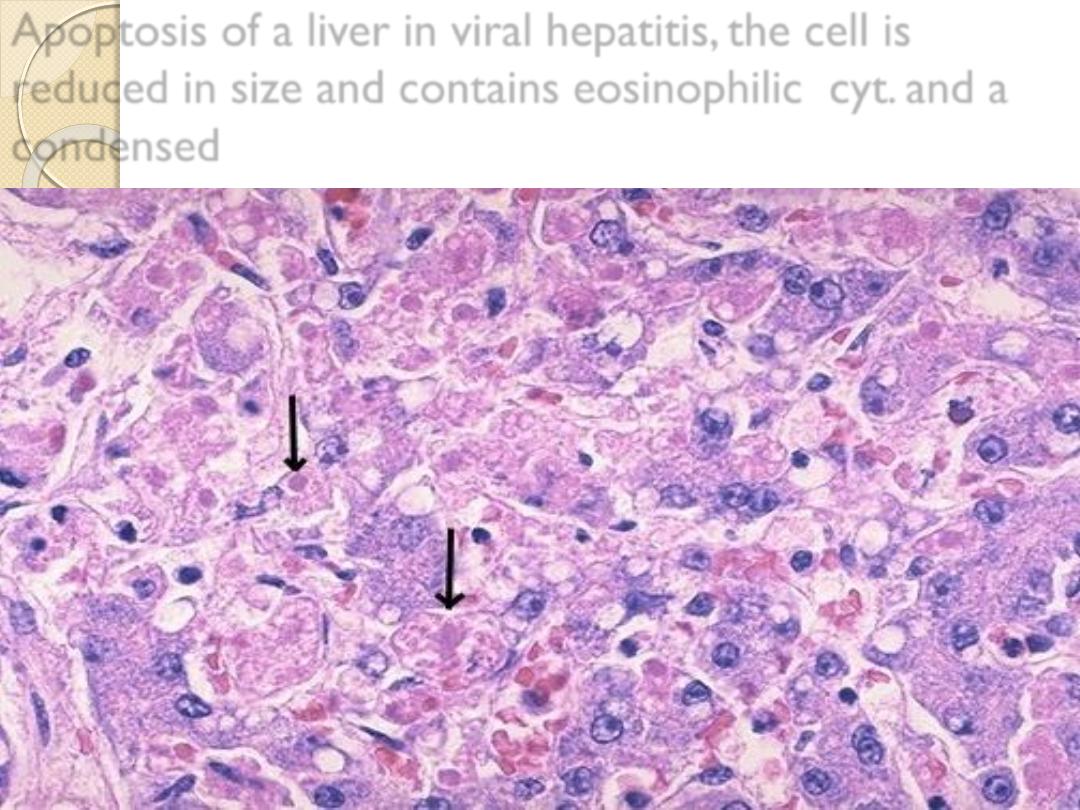
Apoptosis of a liver in viral hepatitis, the cell is
reduced in size and contains eosinophilic cyt. and a
condensed
Apoptotic body appears as dense eosinophilic core

So, failure of cells to undergo apoptosis may result in
undesirable effects that includes:
1-Anomalous development of various organs and
tissues.
2-Progrssive acceleration of tumor growth.
3-Autoimmune diseases e.g. SLE. , Rheumatoid
arthritis ( RA ).
Differences between apoptosis &
necrosis
Apoptosis
Necrosis
Active process
Occur in single cells
Physiological & pathological
No inflammatory reaction
Step-ladder appearance on gel-
electrophoresis for DNA
material
Programmed process
Mechanism;
◦
Gene activation
◦
Caspases activation causing
activation of activate cytoplasmic
endonuclease, proteases &
transglutaminase
Passive process
Affects mass of cells
Always pathological
Stimulate inflammation
Smudge pattern appearance of
DNA material on gel-
electrophoresis
Random process
Mechanism;
◦
ATP depletion
◦
Cell membrane injury
Differences between apoptosis &
necrosis
Apoptosis
Necrosis
Morphology:
◦
Cell shrinkage
◦
Nuclear condensation &
fragmentation
◦
Formation of apoptotic
bodies
◦
Apoptotic bodies engulf
by macrophages
Morphology
◦
Cell swelling
◦
Nuclear changes
(pyknosis, karyorrhexis
& karyolysis)
◦
Eosinophilic cytoplasm
◦
Necrotic area infiltrate
& cleaned by
inflammatory cells

Sub-cellular responses to injury
1/ Cytoskeletal alterations
Defect in cell function
e.g. defect in locomotion or
intracellular translocations.
Accumulations of fibrillar material
e.g. Mallory
body in alcoholic consumption & neurofibrillary tangle in
Alzheimer’s disease .
2/mitochondrial alterations
Increase number of mitochondria in hypertrophy.
decrease number of mitochondria in atrophy.
Mega mitochondria of hepatocytes in alcoholic patient.
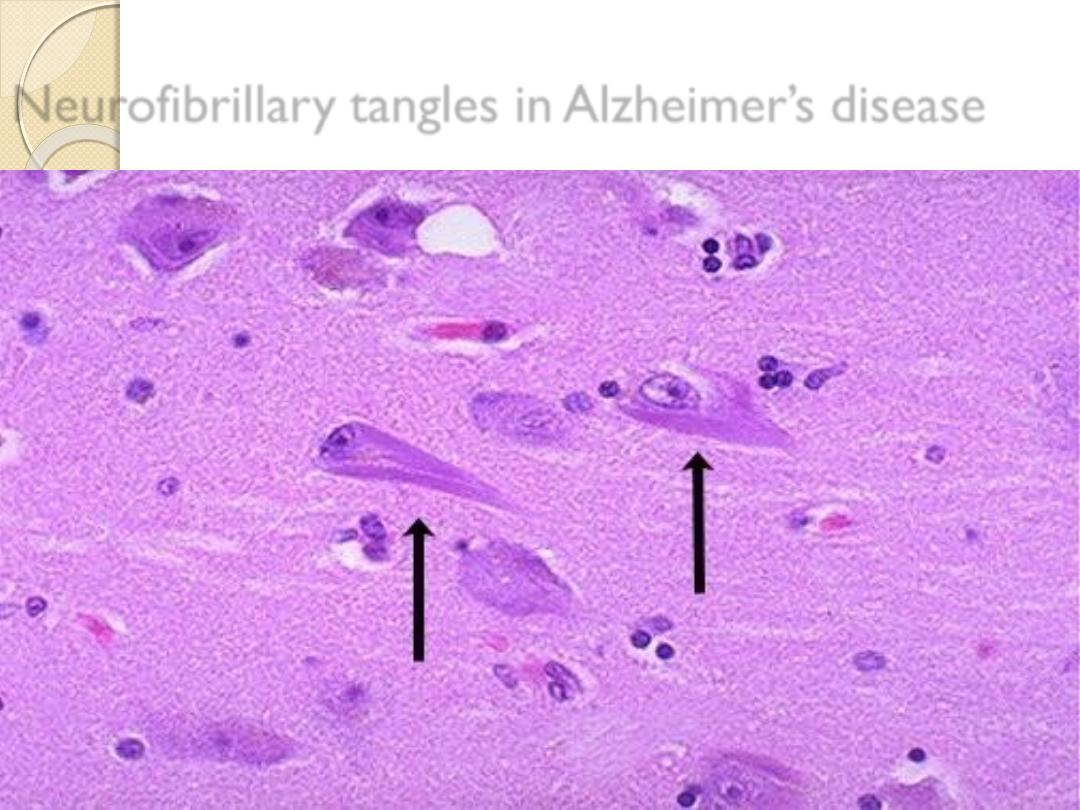
Neurofibrillary tangles in Alzheimer’s disease

3/Smooth endoplasmic reticulum
Increase synthesis of SER in hepatocytes in patients taken
barbiturates drugs
this leads to increase tolerance to these
drugs with time. Therefore; more drug is needed to reach
the therapeutic level.
4/ Lysosomal catabolism
Lysosomes are involved in the breakdown of phagocytosed
material in one of 2 ways:
Heterophagy
: material taken from external environment,
e.g. uptake & digestion of bacteria by neutrophils &
removal of necrotic debris.
Autophagy
: removal of damaged organelles inside the
cells.

Hyaline change
A descriptive term referring to any alteration within the
cells or in the extracellular spaces or structures that gives a
homogenous, glassy-pink appearance
in routine
histological sections stained with H & E.
Example of
intracellular hyaline
◦
Hyaline droplets in PCT of kidney in proteinuria.
◦
Russell bodies in plasma cells.
◦
Alcoholic hyaline in hepatocytes.
◦
Viral inclusion.
Example of
extracellular hyaline
◦
Hyaline arteriolosclerosis.
◦
Amyloid.
◦
Scar.

Fatty changes ( Steatosis)
It’s abnormal accumulation of fat of free
triglyceride
type
within parenchymal cells i.e. in tissue other than
adipose tissue.
Normally fat present in fat depots ( subcutaneous tissue,
pericardium , omentum and mesentry).
It is an example
of reversible cell injury
.
seen often in the
liver
in which fat centrally
metabolized
& to less extend in
heart .

What’s the causes of fatty change??
1-Toxins including alcohol fatty change will appear in the
liver after
6 days
of drinking any amount of alcohol and
disappear after 8 years.
2-Starvation , protein malnutrition & wasting disease
like cancer and tuberculosis.
3-Diabetes mellitus.
4-Oxygen lack (anemia & ischemia).
5-Drugs & chemicals e.g. CCL4 and phosphorus.
6-Obesity.
7- acute fatty liver in pregnancy and Reye’s syndrome
here the defect in mitochondrial oxidation.

Morphology of Fatty liver
Gross features : In the liver mild fatty changes shows no
changes, but with further accumulation the organ enlarges
&
become increasingly yellow, soft & greasy to
touch.
Microscopically : In the early stages there are small fat
vacuoles around the nucleus
(microvesicular steatosis).
With progression the vacuoles fuse together creating large
clear space that displaces the nucleus to the periphery
(macrovesicular steatosis).
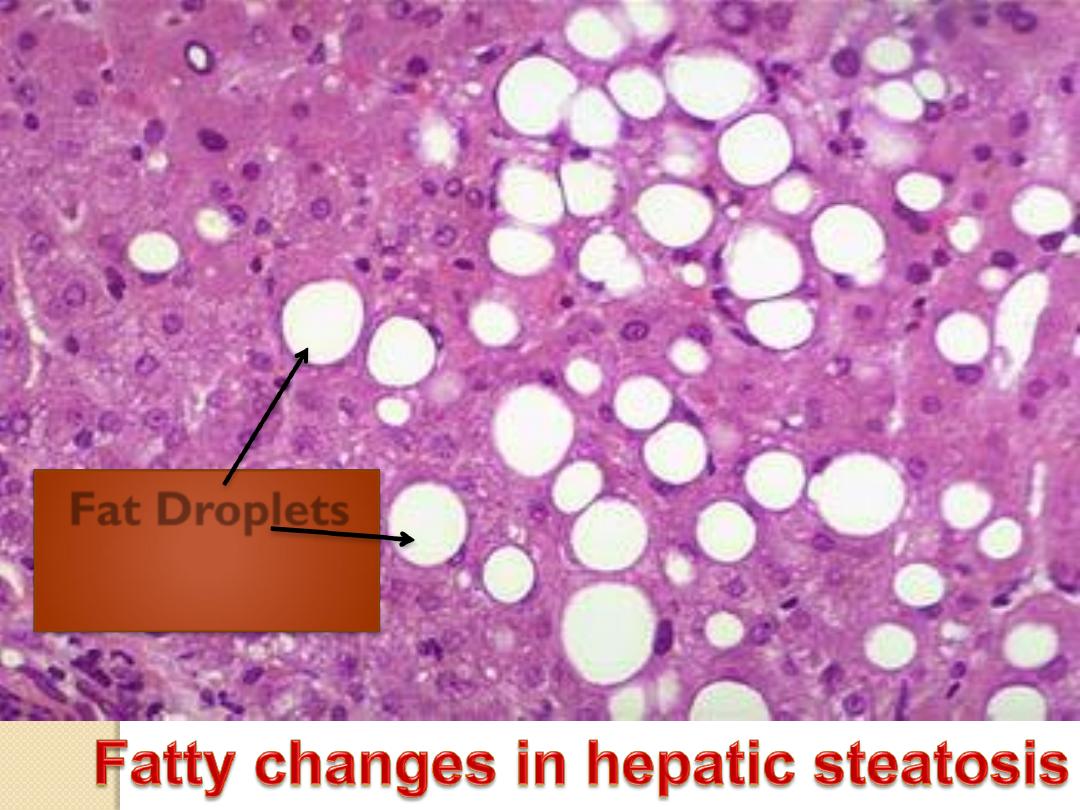
Fat Droplets
The significant of fatty changes depend on
1- the cause.
2-the severity of the accumulation ( mild, moderate
or severe).
Moreover fatty changes it’s
reversible
when the
cause is removed.
Note;
cholesterol deposition; result of
defective catabolism and excessive intake; in
macrophages and smooth muscle cells of vessel
walls in
atherosclerosis
.
Calcifications
We are born with calcium in our
teeth and
bones .
Osteoblasts and odontoblasts fix
calcium and phosphorus , and then
precipitate the products into an organic
matrix ; this is the process of physiologic
biomineralization involving apatite minerals.
As a result of “
ageing
” and disease
states, typically disease states with an
inflammatory component, we calcify
our blood vessels and internal organs
and this is called
“pathological calcification“

Pathological Calcification
This refer to abnormal deposition of calcium salt in
tissues other than bones.
There are two forms of calcification;
1- Dystrophic calcification:
refer to deposition of calcium
in non viable or dying
tissues in the presence of normal serum level of
calcium
with normal calcium metabolism. E.g.
◦
Areas of necrosis (caseous , coagulative or fat
necrosis).
◦
Wall of artery in atherosclerosis.
◦
Aging or disease of the heart valve.
◦
Dead parasites & their ova.
Of calcification
Pathogenesis
It is not well known, it could be due to one of the
followings:
1-Increase in the pH of the tissue i.e. become
alkaline.
2-Release of alkaline phosphatase which
stimulates deposition of calcium.
3-The presence of cellular product which acts
as a nucleus that stimulates the deposition of
calcium around it.
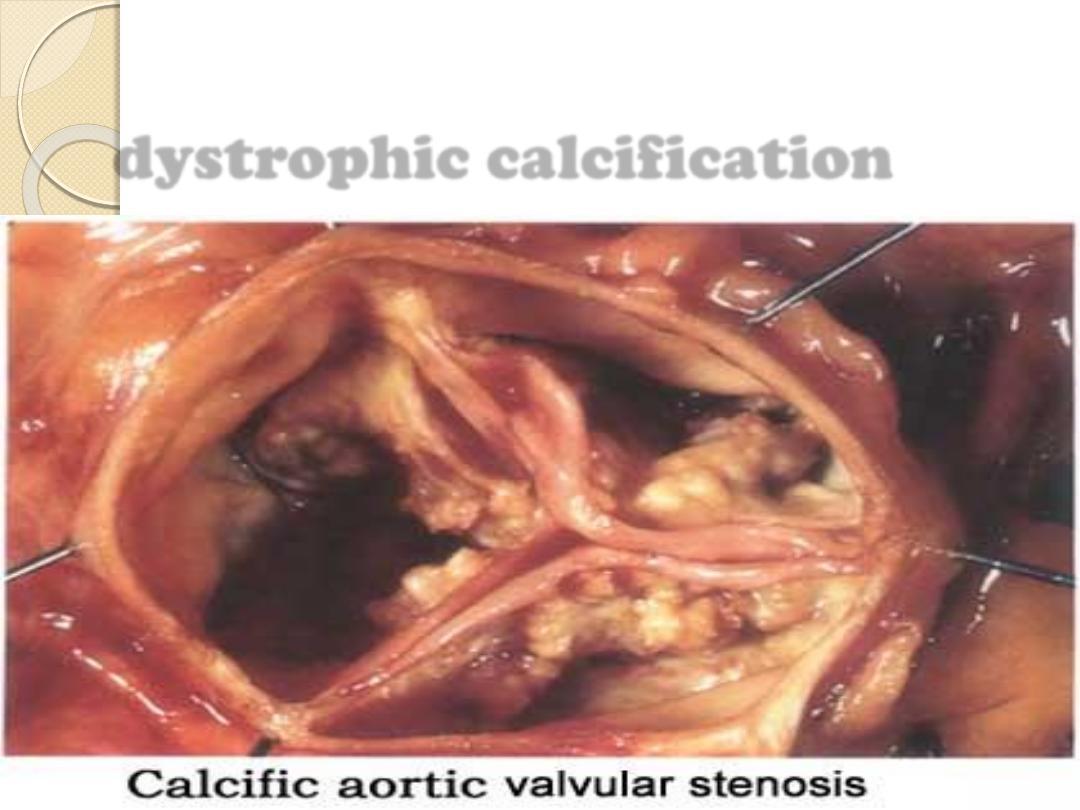
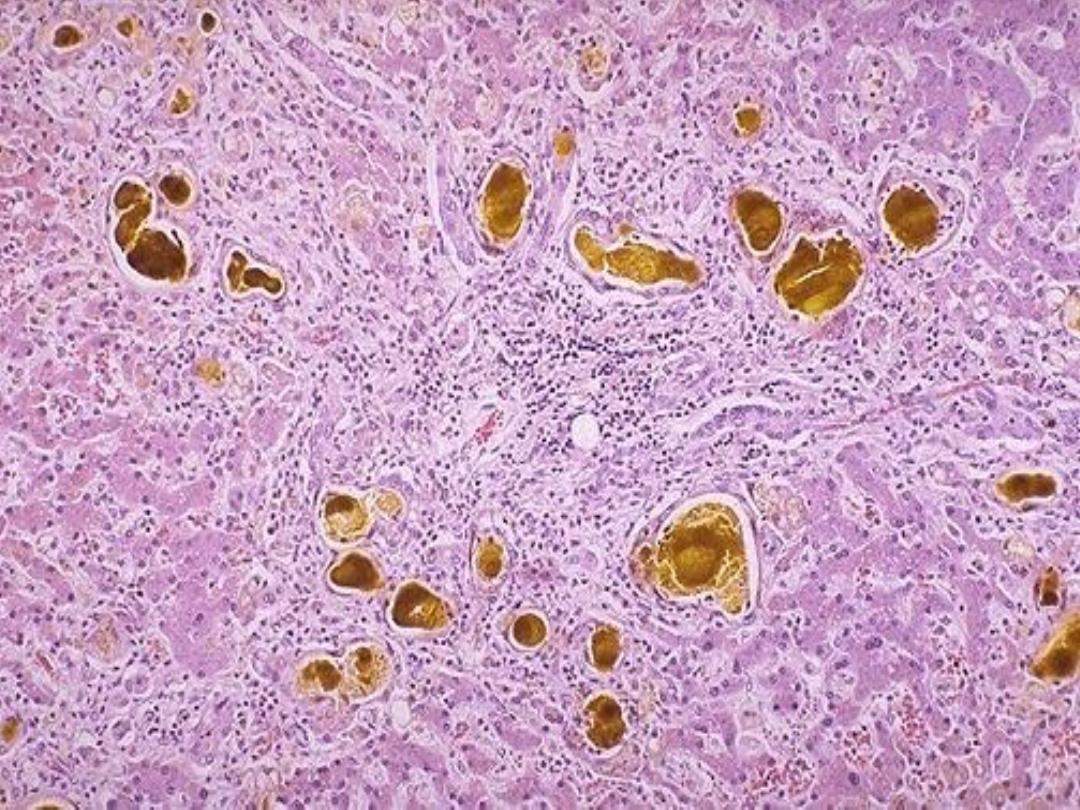
dystrophic calcification
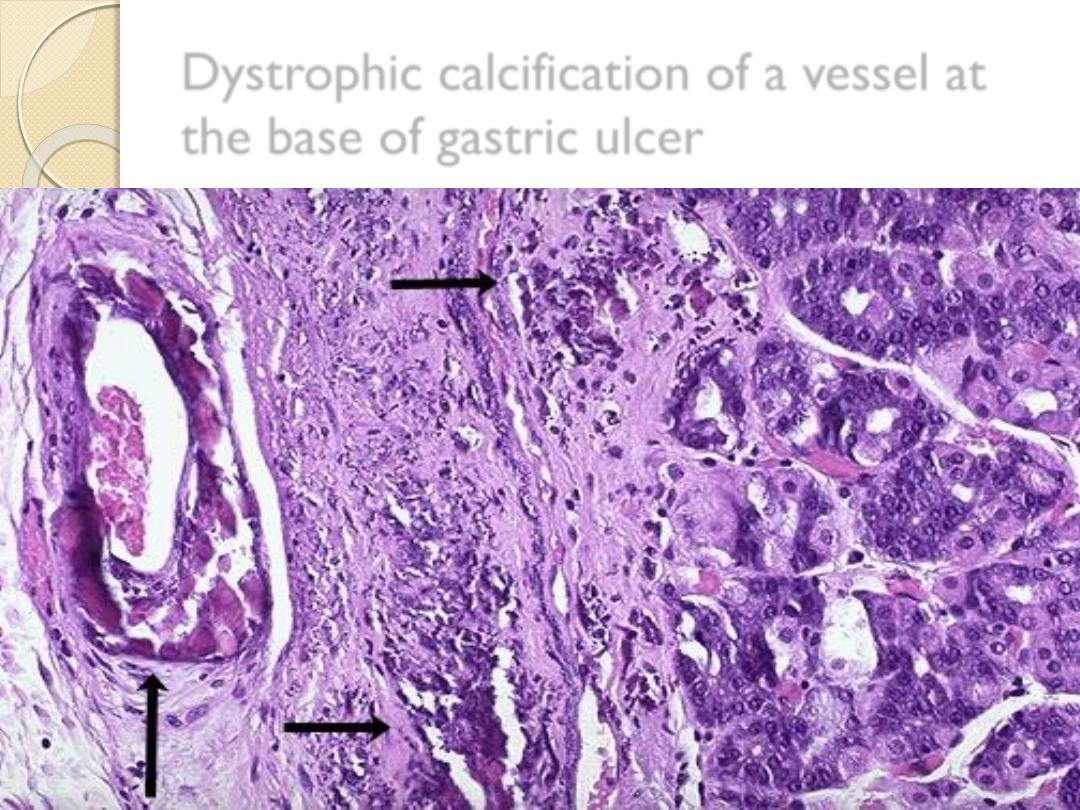
Dystrophic calcification of a vessel at
the base of gastric ulcer

Dystrophic calcification of dead
parasite in the lung

2-Metastatic calcification:
refer to deposition of calcium
in viable tissue in the
presence of high serum calcium level.
Causes of hypercalcaemia:
◦
Hyperparathyrodisum.
◦
Vitamin D intoxication.
◦
Sarcoidosis.
◦
Metastatic cancer to the bone.
◦
Some other non metastatic cancer.
Organ affected are:
kidneys, stomach, lungs , systemic and
pulmonary arteries.
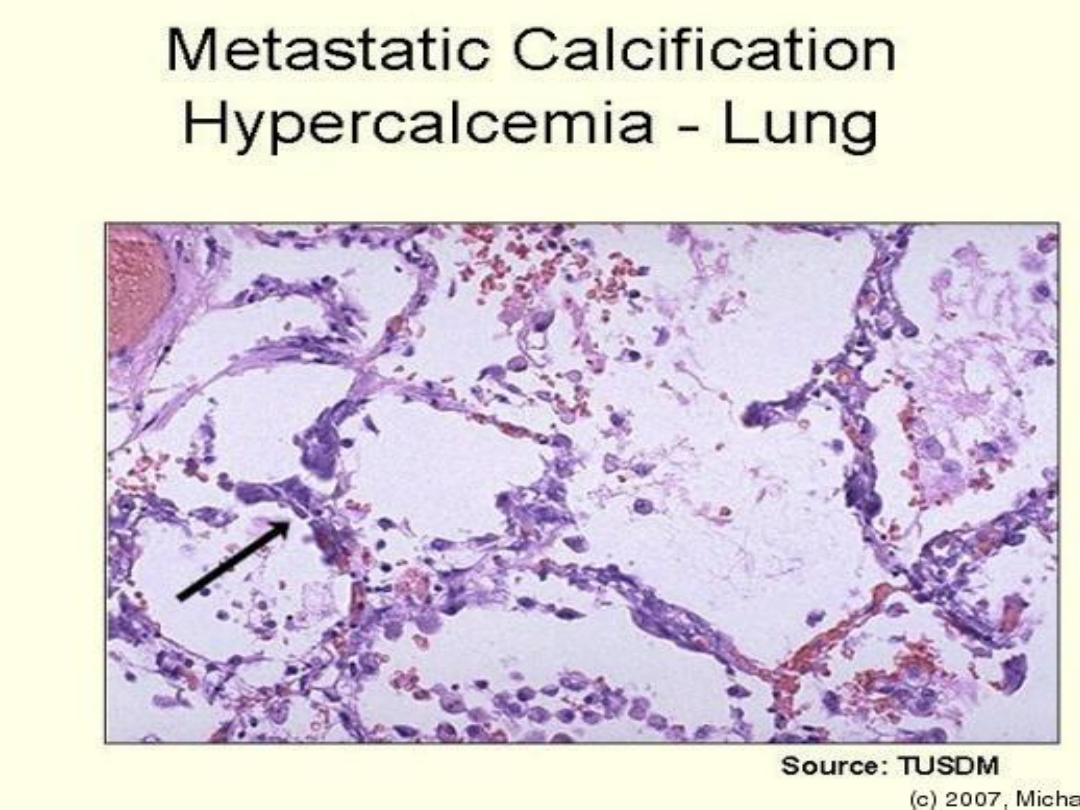
metastatic calcification

Colored substances (pigments)
A-Exogenous
e.g. Carbon (coal dust), accumulation of carbon pigment in
the lung give it black color called
(anthracosis).
Tattooing
the pigment inoculated is taken by
dermal
macrophages.
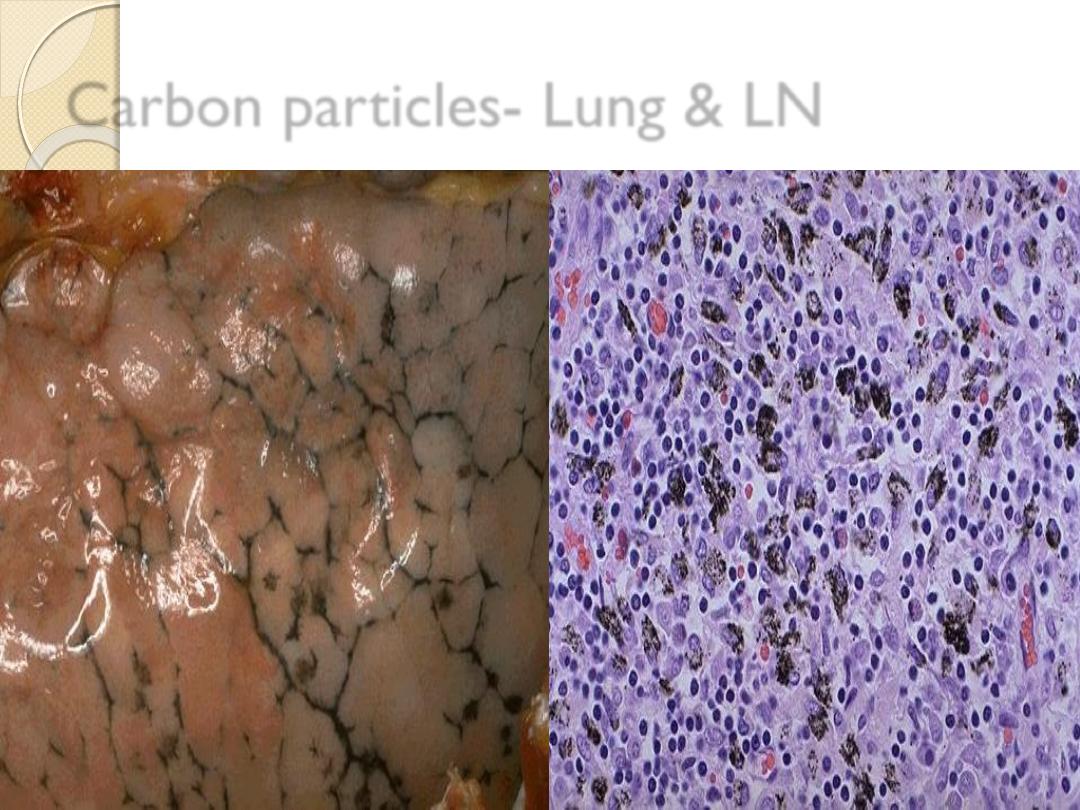
Carbon particles- Lung & LN

B-Endogenous pigments:
1-Lipofuscin (lipochrom pigment), is a yellow brown,
intracytoplasmic pigment, which is seen in the cells
undergoing slow atrophy.
It represents
residue of oxidized lipid derived from
digested membrane of organelles
◦
1-Particularly prominent in the cells of the liver &
heart of the elderly (brown atrophy of the heart).
It is called wear & tear pigment
◦
2-Patein with sever malnutrition and cancer cachexia.
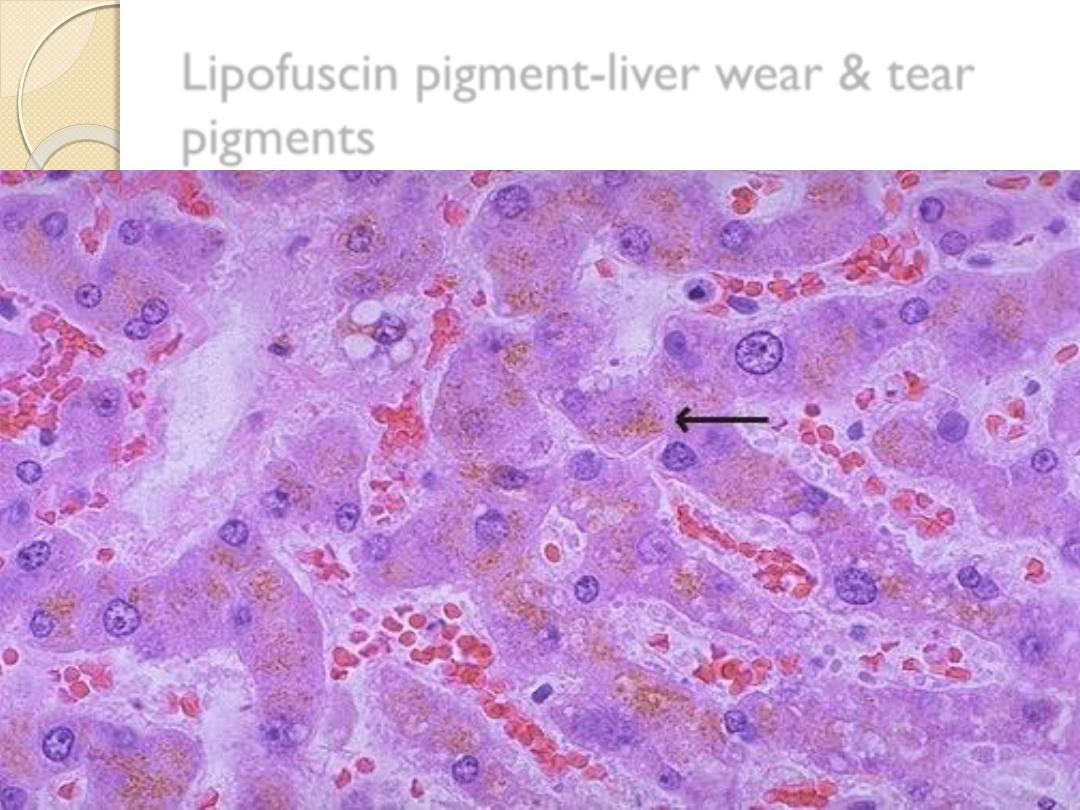
Lipofuscin pigment-liver wear & tear
pigments

2-Melanin:
This is an endogenous non-hemoglobin-derived brown
black pigment.
The skin pigment is produced by the
oxidation of tyrosine through the help of tyrosinase
enzyme within the melanocytes.
Lesions associated with melanocytes are
◦
Moles (nevi) …….benign lesion.
◦
Melanoma………..Malignant.

3-Bilirubin:
It is a normal major
pigment of bile
, which is derived
from the
heme portion of hemoglobin
.
The conversion to bile occur in
the liver
.
Jaundice: result from excess of bilirubin pigment.


4-Hemosidrin:
It is
a hemoglobin-derived, golden-yellow to
brown granules.
Excess iron in the body causes
hemosiderin
to
accumulate within the cell. Excess deposition is termed as
hemosiderosis
which is either localized or systemic.
Special stain for iron is
Prussian blue or Perl’s stain.
Localized hemosiderosis: result from local hemorrhage
e.g. bruise, cerebral hemorrhage.
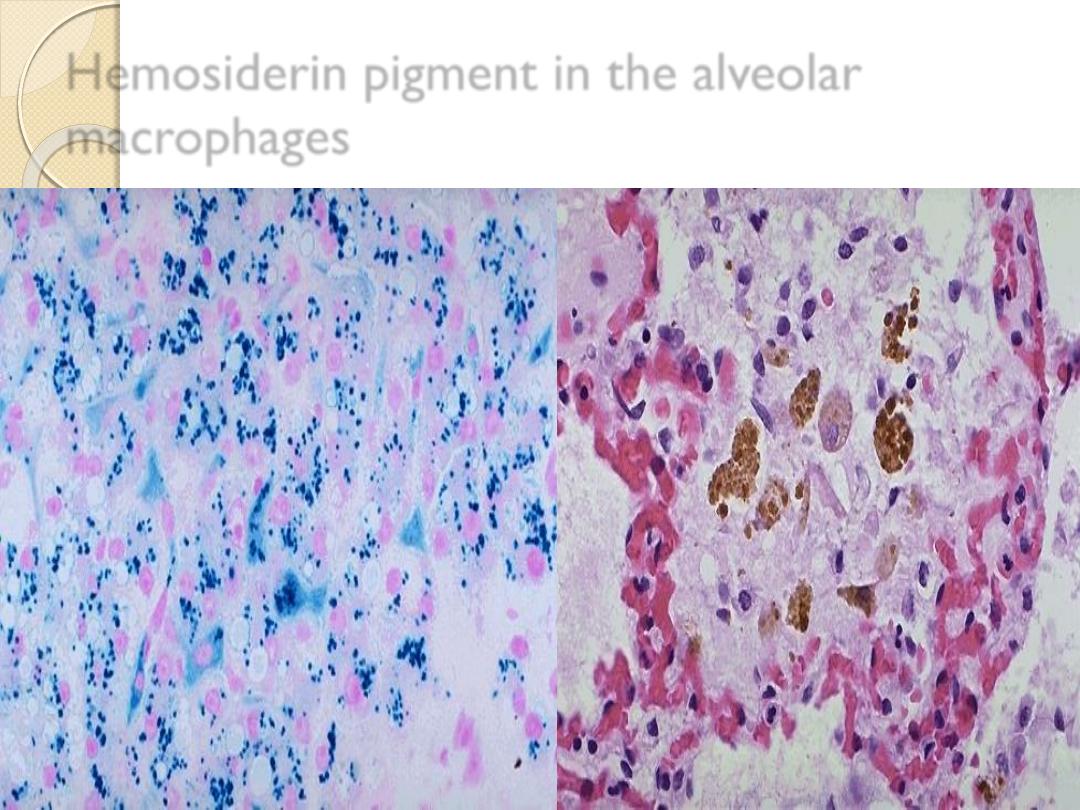
Hemosiderin pigment in the alveolar
macrophages

Systemic hemosiderosis:
occur whenever there is
systemic iron overload, this is associated with
◦
1-Increased iron absorption.
◦
2-Impaired utilization of iron.
◦
3-Hemolytic anemia.
◦
4-Excessive blood transfusion.
In systemic hemosiderosis, hemosiderin accumulate
first
in the reteculoendothelial cells,
with progression the
accumulation cause tissue damage, by the deposition of the
iron pigment in the main
parenchymal cells
in a disease
called
hemochromatosis.

Hemochromatosis
Predominantly affects male
40-60 years
Idiopathic form transmitted as autosomal recessive trait
There is 0.5 gm of iron accumulated in the body /year
There is lack of regulation of iron absorption from GIT
Liver cirrhosis
Diabetes mellitus
Skin pigmentation causing bronzed diabetes
Atrophy of the testes
Liver cancer
Cellular Aging
It is the result of a progressive decline in the proliferative
capacity and life span of cells and the effects of continuous
exposure to exogenous factors that cause accumulation
of cellular and molecular damage .
The mechanisms for cellular aging
.
1- DNA damage
2-decreased cellular replication
3-reduced regenerative capacity of tissue stem cells.
4-Accumulation of metabolic damage.
Cellular aging
Cellular aging is
multifactorial
1- an endogenous molecular program.
2- continuous exposure through out life to adverse
exogenous influences.
It ‘s called
wear and tear
process, in cell aging
molecular injury to cells exceeds their repair
capacity thus accelerating the aging process.
Favored theory for cell aging is
the progressive
effects of free radicals through out life.

Thank You
